Abstract
Aims/hypothesis
Obesity increases the risk of developing type 2 diabetes mellitus, characterised by impaired insulin-mediated glucose uptake in peripheral tissues. Liver X receptor (LXR) is a positive regulator of adipocyte glucose transport in murine models and a possible target for diabetes treatment. However, the levels of LXRα are increased in obese adipose tissue in humans. We aimed to investigate the transcriptome of LXR and the role of LXR in the regulation of glucose uptake in primary human adipocytes.
Methods
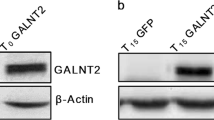
The insulin responsiveness of human adipocytes differentiated in vitro was characterised, adipocytes were treated with the LXR agonist GW3965 and global transcriptome profiling was determined by microarray, followed by quantitative RT-PCR (qRT-PCR), western blot and ELISA. Basal and insulin-stimulated glucose uptake was measured and the effect on plasma membrane translocation of glucose transporter 4 (GLUT4) was assayed.
Results
LXR activation resulted in transcriptional suppression of several insulin signalling genes, such as AKT2, SORBS1 and CAV1, but caused only minor changes (<15%) in microRNA expression. Activation of LXR impaired the plasma membrane translocation of GLUT4, but not the expression of its gene, SLC2A4. LXR activation also diminished insulin-stimulated glucose transport and lipogenesis in adipocytes obtained from overweight individuals. Furthermore, AKT2 expression was reduced in obese adipose tissue, and AKT2 and SORBS1 expression was inversely correlated with BMI and HOMA index.
Conclusions/interpretation
In contrast to murine models, LXR downregulates insulin-stimulated glucose uptake in human adipocytes from overweight individuals. This could be due to suppression of Akt2, c-Cbl-associated protein and caveolin-1. These findings challenge the idea of LXR as a drug target in the treatment of diabetes.





Similar content being viewed by others
Abbreviations
- 22-R-HC:
-
22-R-Hydroxycholesterol
- CAP:
-
c-Cbl associated protein
- CAV1:
-
Caveolin 1
- FAS:
-
Fatty acid synthase
- GLUT4:
-
Glucose transporter 4
- hMSC:
-
Human mesenchymal stem cell
- HOMA-IR:
-
HOMA of insulin resistance
- LXR:
-
Liver X receptor
- miRNA:
-
MicroRNA
- PM:
-
Plasma membrane
- qRT-PCR:
-
Quantitative real-time RT-PCR
- RXR:
-
Retinoic X receptor
- SAM:
-
Significance analysis of microarray
- SGBS:
-
Simpson–Golabi–Behmel syndrome
References
Guilherme A, Virbasius JV, Puri V, Czech MP (2008) Adipocyte dysfunctions linking obesity to insulin resistance and type 2 diabetes. Nat Rev Mol Cell Biol 9:367–377
Leto D, Saltiel AR (2012) Regulation of glucose transport by insulin: traffic control of GLUT4. Nat Rev Mol Cell Biol 13:383–396
Chiang SH, Baumann CA, Kanzaki M et al (2001) Insulin-stimulated GLUT4 translocation requires the CAP-dependent activation of TC10. Nature 410:944–948
Miura A, Sajan MP, Standaert ML et al (2003) Cbl PYXXM motifs activate the P85 subunit of phosphatidylinositol 3-kinase, Crk, atypical protein kinase C, and glucose transport during thiazolidinedione action in 3T3/L1 and human adipocytes. Biochemistry 42:14335–14341
Yamamoto M, Toya Y, Schwencke C, Lisanti MP, Myers MG Jr, Ishikawa Y (1998) Caveolin is an activator of insulin receptor signaling. J Biol Chem 273:26962–26968
Olson AL, Pessin JE (1996) Structure, function, and regulation of the mammalian facilitative glucose transporter gene family. Annu Rev Nutr 16:235–256
Trajkovski M, Hausser J, Soutschek J et al (2011) MicroRNAs 103 and 107 regulate insulin sensitivity. Nature 474:649–653
Baranowski M (2008) Biological role of liver X receptors. J Physiol Pharmacol 59(Suppl 7):31–55
Dahlman I, Nilsson M, Jiao H et al (2006) Liver X receptor gene polymorphisms and adipose tissue expression levels in obesity. Pharmacogenet Genomics 16:881–889
Dahlman I, Nilsson M, Gu HF et al (2009) Functional and genetic analysis in type 2 diabetes of liver X receptor alleles—a cohort study. BMC Med Genet 10:27
Solaas K, Legry V, Retterstol K et al (2010) Suggestive evidence of associations between liver X receptor beta polymorphisms with type 2 diabetes mellitus and obesity in three cohort studies: HUNT2 (Norway), MONICA (France) and HELENA (Europe). BMC Med Genet 11:144
Ross SE, Erickson RL, Gerin I et al (2002) Microarray analyses during adipogenesis: understanding the effects of Wnt signaling on adipogenesis and the roles of liver X receptor alpha in adipocyte metabolism. Mol Cell Biol 22:5989–5999
Laffitte BA, Chao LC, Li J et al (2003) Activation of liver X receptor improves glucose tolerance through coordinate regulation of glucose metabolism in liver and adipose tissue. Proc Natl Acad Sci U S A 100:5419–5424
Dalen KT, Ulven SM, Bamberg K, Gustafsson JA, Nebb HI (2003) Expression of the insulin-responsive glucose transporter GLUT4 in adipocytes is dependent on liver X receptor alpha. J Biol Chem 278:48283–48291
Griesel BA, Weems J, Russell RA, Abel ED, Humphries K, Olson AL (2010) Acute inhibition of fatty acid import inhibits GLUT4 transcription in adipose tissue, but not skeletal or cardiac muscle tissue, partly through liver X receptor (LXR) signaling. Diabetes 59:800–807
Commerford SR, Vargas L, Dorfman SE et al (2007) Dissection of the insulin-sensitizing effect of liver X receptor ligands. Mol Endocrinol 21:3002–3012
Fernandez-Veledo S, Vila-Bedmar R, Nieto-Vazquez I, Lorenzo M (2009) c-Jun N-terminal kinase 1/2 activation by tumor necrosis factor-alpha induces insulin resistance in human visceral but not subcutaneous adipocytes: reversal by liver X receptor agonists. J Clin Endocrinol Metab 94:3583–3593
Fernandez-Veledo S, Nieto-Vazquez I, de Castro J et al (2008) Hyperinsulinemia induces insulin resistance on glucose and lipid metabolism in a human adipocytic cell line: paracrine interaction with myocytes. J Clin Endocrinol Metab 93:2866–2876
Hessvik NP, Bakke SS, Smith R et al (2012) The liver X receptor modulator 22(S)-hydroxycholesterol exerts cell-type specific effects on lipid and glucose metabolism. J Steroid Biochem Mol Biol 128:154–164
Arner E, Mejhert N, Kulyte A et al (2012) Adipose tissue microRNAs as regulators of CCL2 production in human obesity. Diabetes 61:1986–1993
van Harmelen V, Skurk T, Hauner H (2005) Primary culture and differentiation of human adipocyte precursor cells. Methods Mol Med 107:125–135
Dicker A, Le Blanc K, Astrom G et al (2005) Functional studies of mesenchymal stem cells derived from adult human adipose tissue. Exp Cell Res 308:283–290
Rodriguez AM, Pisani D, Dechesne CA et al (2005) Transplantation of a multipotent cell population from human adipose tissue induces dystrophin expression in the immunocompetent mdx mouse. J Exp Med 201:1397–1405
Zaragosi LE, Ailhaud G, Dani C (2006) Autocrine fibroblast growth factor 2 signaling is critical for self-renewal of human multipotent adipose-derived stem cells. Stem Cells 24:2412–2419
Rodbell M (1964) Metabolism of isolated fat cells. I. Effects of hormones on glucose metabolism and lipolysis. J Biol Chem 239:375–380
Collins JL, Fivush AM, Watson MA et al (2002) Identification of a nonsteroidal liver X receptor agonist through parallel array synthesis of tertiary amines. J Med Chem 45:1963–1966
Stenson BM, Ryden M, Steffensen KR et al (2009) Activation of liver X receptor regulates substrate oxidation in white adipocytes. Endocrinology 150:4104–4113
Gerin I, Dolinsky VW, Shackman JG et al (2005) LXRbeta is required for adipocyte growth, glucose homeostasis, and beta cell function. J Biol Chem 280:23024–23031
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25:402–408
Lofgren P, van Harmelen V, Reynisdottir S et al (2000) Secretion of tumor necrosis factor-alpha shows a strong relationship to insulin-stimulated glucose transport in human adipose tissue. Diabetes 49:688–692
Arner P, Engfeldt P (1987) Fasting-mediated alteration studies in insulin action on lipolysis and lipogenesis in obese women. Am J Physiol 253:E193–E201
Elmensdorf JS (2003) Fractionation analysis of the subcellular distribution of GLUT-4 in 3T3-L1 adipocytes. In: Özcan S (ed) Diabetes mellitus: methods and protocols. Humana Press, Totowa, pp 105–111
Zhang B, Kirov S, Snoddy J (2005) WebGestalt: an integrated system for exploring gene sets in various biological contexts. Nucleic Acids Res 33:W741–W748
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Grefhorst A, van Dijk TH, Hammer A et al (2005) Differential effects of pharmacological liver X receptor activation on hepatic and peripheral insulin sensitivity in lean and ob/ob mice. Am J Physiol Endocrinol Metab 289:E829–E838
Kotokorpi P, Ellis E, Parini P et al (2007) Physiological differences between human and rat primary hepatocytes in response to liver X receptor activation by 3-[3-[N-(2-chloro-3-trifluoromethylbenzyl)-(2,2-diphenylethyl)amino]propyloxy]phe nylacetic acid hydrochloride (GW3965). Mol Pharmacol 72:947–955
Pehkonen P, Welter-Stahl L, Diwo J et al (2012) Genome-wide landscape of liver X receptor chromatin binding and gene regulation in human macrophages. BMC Genomics 13:50
Stulnig TM, Steffensen KR, Gao H et al (2002) Novel roles of liver X receptors exposed by gene expression profiling in liver and adipose tissue. Mol Pharmacol 62:1299–1305
Kulyte A, Pettersson AT, Antonson P et al (2011) CIDEA interacts with liver X receptors in white fat cells. FEBS Lett 585:744–748
Sun D, Zhang J, Xie J, Wei W, Chen M, Zhao X (2012) MiR-26 controls LXR-dependent cholesterol efflux by targeting ABCA1 and ARL7. FEBS Lett 586:1472–1479
George S, Rochford JJ, Wolfrum C et al (2004) A family with severe insulin resistance and diabetes due to a mutation in AKT2. Science 304:1325–1328
Lin WH, Chiu KC, Chang HM, Lee KC, Tai TY, Chuang LM (2001) Molecular scanning of the human sorbin and SH3-domain-containing-1 (SORBS1) gene: positive association of the T228A polymorphism with obesity and type 2 diabetes. Hum Mol Genet 10:1753–1760
Kim CA, Delepine M, Boutet E et al (2008) Association of a homozygous nonsense caveolin-1 mutation with Berardinelli-Seip congenital lipodystrophy. J Clin Endocrinol Metab 93:1129–1134
Zhou QL, Park JG, Jiang ZY et al (2004) Analysis of insulin signalling by RNAi-based gene silencing. Biochem Soc Trans 32:817–821
Tan SX, Ng Y, Meoli CC et al (2012) Amplification and demultiplexing in insulin-regulated Akt protein kinase pathway in adipocytes. J Biol Chem 287:6128–6138
Katz A, Udata C, Ott E et al (2009) Safety, pharmacokinetics, and pharmacodynamics of single doses of LXR-623, a novel liver X-receptor agonist, in healthy participants. J Clin Pharmacol 49:643–649
Stenson BM, Ryden M, Venteclef N et al (2011) Liver X receptor (LXR) regulates human adipocyte lipolysis. J Biol Chem 286:370–379
Arner P (2005) Human fat cell lipolysis: biochemistry, regulation and clinical role. Best Pract Res Clin Endocrinol Metab 19:471–482
Kase ET, Wensaas AJ, Aas V et al (2005) Skeletal muscle lipid accumulation in type 2 diabetes may involve the liver X receptor pathway. Diabetes 54:1108–1115
Kase ET, Thoresen GH, Westerlund S, Hojlund K, Rustan AC, Gaster M (2007) Liver X receptor antagonist reduces lipid formation and increases glucose metabolism in myotubes from lean, obese and type 2 diabetic individuals. Diabetologia 50:2171–2180
Acknowledgements
The excellent technical assistance of E. Sjölin, K. Wåhlén, E. Dungner, B.-M. Leijonhufvud, Y. Widlund and K. Hertel (Department of Medicine Huddinge, Karolinska Institutet, Sweden) is greatly appreciated. We also thank T. Skurk (Else Kröner-Fresenius-Centre for Nutritional Medicine, Technical University of Munich, Germany) for advice.
Funding
This study was supported by the Swedish Research Council, NovoNordisk, Swedish Diabetes Association, Swedish Heart-Lung Foundation, Karolinska Institutet, SRP Diabetes programme, Åke Wiberg Foundation, Magnus Bergvalls Foundation, Tore Nilsson Foundation, NordForsk (SYSDIET-070014) and NWO Rubicon (825.07.025).
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
JL and AMLP designed the study. AMLP, BMS, JK, JL, NM, DPA, ID and PA performed experiments, acquired data and/or performed data analysis and interpretation. SLC, AMLP, JL and JK carried out cell system characterisations. AMLP, JK, JL, SLC, GÅ and AVC designed, performed and analysed method development experiments. AP and JL drafted the manuscript. All authors revised the manuscript critically and approved the final version.
Author information
Authors and Affiliations
Corresponding authors
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Methods
(PDF 222 kb)
ESM Table 1
(PDF 152 kb)
ESM Table 2
(PDF 145 kb)
ESM Fig. 1
(PDF 89 kb)
ESM Fig. 2
(PDF 87 kb)
ESM Fig. 3
(PDF 134 kb)
ESM Fig. 4
(PDF 83 kb)
ESM Fig. 5
(PDF 90 kb)
ESM Fig. 6
(PDF 96 kb)
Rights and permissions
About this article
Cite this article
Pettersson, A.M.L., Stenson, B.M., Lorente-Cebrián, S. et al. LXR is a negative regulator of glucose uptake in human adipocytes. Diabetologia 56, 2044–2054 (2013). https://doi.org/10.1007/s00125-013-2954-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-013-2954-5