Abstract
Background
The treatment of urinary tract infection (UTI), the most common bacterial infection in most Western countries, is a global clinical and economic issue. Trimethoprim-sulfamethoxazole (TMP-SMX) and nitrofurantoin are the two drugs currently recommended in clinical guidelines in Israel for uncomplicated UTI in women.
Objectives
This study evaluates physician preferences for treatment and adherence to guidelines.
Method
Data were derived from the electronic records of Leumit Health Fund, one of four health management organizations in Israel. Non-pregnant women aged 18–75 years with a diagnosis of acute cystitis or UTI without risk factors for complicated UTI who were empirically treated with antibiotics from January 2001 to June 2002 were identified. The final sample comprised 7738 physician–patient encounters. Physician prescription behavior was analyzed by evaluating the proportion of treatments with each individual drug. A binary regression model was implemented to identify factors associated with suboptimal adherence to the guidelines.
Results
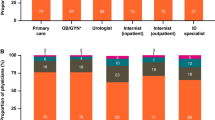
TMP-SMX was the most frequently prescribed drug (25.81%), followed by nitrofurantoin (14.71%), for a 40.52% rate of adherence to the guidelines [95% confidence interval (CI)=39.42, 41.61]. Drugs from the fluoroquinolone family were prescribed in 22.82% of cases. Prescription behavior was also influenced by non-clinical, non-pharmacological factors, such as physician specialty, geographic setting and patient age.
Conclusions
The majority of cases of UTI in the present study were not treated according to the current guidelines. Fluoroquinolones, though not recommended and relatively costly, were prescribed extensively. These results highlight the necessity for a remedial education program within the health care system designed to improve adherence to the guidelines for the treatment of UTI in women. As this issue is of global importance, this evaluation may serve as a model for similar studies in other settings or countries.
Similar content being viewed by others
References
Nicolle LE (2001) Epidemiology of urinary tract infection. Infect Med 18:153–162
Peterson GM, Stanton LA, Bergin JK, Chapman GA (1997) Improving the prescribing of antibiotics for urinary tract infection. J Clin Pharm Ther 22:147–153
Hooton TM, Stamm WE (1997) Diagnosis and treatment of uncomplicated urinary tract infection. Infect Dis Clin North Am 11:551–581
Saint S, Scholes D, Fihn SD, Farrell RG, Stamm WE (1999) The effectiveness of a clinical practice guideline for the management of presumed uncomplicated urinary tract infection in women. Am J Med 106:636–641
Avorn J, Solomon DH (2000) Cultural and economic factors that (mis)shape antibiotic use: the nonpharmacologic basis of therapeutics. Ann Intern Med 133:128–135
Berg AO (1991) Variation among family physicians' management strategies for lower urinary tract infection in women: a report from the Washington Family Physicians Collaborative Research Network. J Am Board Fam Pract 4:327–330
Komaroff AL, Pass TM, McCue JD, Cohen AB, Hendricks TM, Friedland G (1978) Management strategies for urinary and vaginal infections. Arch Intern Med 138:1069–1973
Wigton RS, Longenecker JC, Bryan TJ, Parenti C, Flach SD, Tape TG (1999) Variation by specialty in the treatment of urinary tract infection in women. J Gen Intern Med 14:491–494
Huang ES, Stafford RS (2002) National patterns in the treatment of urinary tract infections in women by ambulatory care physicians. Arch Intern Med 162:41–47
Lambert BL, Salmon JW, Stubbings J, Gilomen-Study G, Valuck RJ, Kezlarian K (1997) Factors associated with antibiotic prescribing in a managed care setting: an explanatory investigation. Soc Sci Med 45:1767–1779
Gupta K, Hooton TM, Stamm WE (2001) Increasing antimicrobial resistance and the management of uncomplicated community acquired urinary tract infections. Ann Intern Med 135:41–50
Gupta K, Scholes D, Stamm WE (1999) Increasing prevalence of antimicrobial resistance among uropathogens causing acute uncomplicated cystitis in women. JAMA 281:736–738
Stamm WE (2002) Scientific and clinical challenges in the management of urinary tract infections. Am J Med 113:1S–4S
McGavock H (2002) Editorial. Pharmacoepidemiol Drug Saf 11:407–408
Hawkes CA (2000) Antibiotic resistance: a clinician's perspective. Military Med 165[Suppl 2]:43–45
Stamm WE, Hooton TM (1993) Management of urinary tract infections in adults. N Engl J Med 329:1328–1334
National Guidelines Clearinghouse. (2002)http://www.guidelines.gov/FRAMESETS/guidelines_fs.asp?guideline=001510&Search_string=uti
Warren JW, Abrutyn E, Hebel JR, Johnson JR, Schaeffer AJ, Stamm W (1999) Guidelines for antimicrobial treatment of uncomplicated acute bacterial cystitis and acute pyelonephritis in women. Clin Infect Dis 29:745–758
Hooton TM, Levy SB (2002) Confronting the antibiotic resistance crisis: making appropriate therapeutic decisions in community medical practice.http://www.medscape.com/viewprogram/618_pnt
Chen FJ, McDonald LC, Ho M, Lo HJ (2001) Molecular epidemiology of ciprofloxacin reduced susceptible Escherichia coli: a herald for emerging resistance (abstract 2113). Program and abstracts of the 41st Interscience Conference on Antimicrobial Agents and Chemotherapy; 16–19 December 2001, Chicago, Illinois
Karlowsky JA (2002) E. coli resistance to ciprofloxacin growing incrementally each year. Antimicrob Agents Chemother. 46:2540–2545
Raz R, Okev N, Kennes Y, Gilboa A, Lavi I, Bisharat N (2000) Demographic characteristics of patients with community acquired bacteriuria and susceptibility of urinary pathogens to antimicrobials in northern Israel. Israel Med Assoc J 2:426–429
Raz R, Chazan B, Kennes Y, Colodner E, Rottensterich E, Dan M, Lavi I, Stamm W (2002) Empiric use of trimethoprim-sulfamethoxazole (TMP-SMX) in the treatment of women with uncomplicated urinary tract infections, in a geographical area with a high prevalence of TMP-SMX-resistant uropathogens. Clin Infect Dis 34:1165–1169
Clinical guidelines for the treatment of common infectious diseases in the community. "General Health Services" Health Services, November 2000
Woolf SH, Hutchinson A, Eccles M, Grimshaw J (1999) Potential benefits, limitations, and harms of clinical guidelines. BMJ 318:527–530
Sarrell ME, Madelberg A, Cohen HA, Kahan E (2002) Compliance of primary care doctors with asthma guidelines and related education programs: the employment factor. IMAJ 4:403–406
Lomas J, Anderson GM, Domnick-Pierre K, Vayda E, Enkin MW, Hannah WJ (1989) Do practice guidelines guide practice? The effect of a consensus statement on the practice of physicians. N Engl J Med 321:1306–1311
Woolf SH (1993) Practice guidelines: a new reality in medicine, III: impact on patient care. Arch Intern Med 153:2646–2655
Hayward RSA (1997) Clinical practice guidelines on trial. CMAJ 156:1725–1727
Huang ES, Stafford RS (2002) National patterns in the treatment of urinary tract infections in women by ambulatory care physicians. Arch Intern Med 162:41–47
Acknowledgements
The authors wish to thank Mr. Etzion Yatsiv, director of the Leumit Health Fund information system, for his kind cooperation; Mr. Shimon Sister and Dr. Amir Fruman for their assistance in programming the database used to identify the cases; and Mrs. Bella Adler for her guidance in the statistical analysis. The authors also wish to thank Mrs. Gloria Ginzach and Mrs. Marian Propp for their editorial and secretarial assistance. This study is part of Natan R. Kahan's Ph.D. dissertation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kahan, E., Kahan, N.R. & Chinitz, D.P. Urinary tract infection in women—physician's preferences for treatment and adherence to guidelines: a national drug utilization study in a managed care setting. Eur J Clin Pharmacol 59, 663–668 (2003). https://doi.org/10.1007/s00228-003-0673-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-003-0673-4