Abstract
A nuclear protein, 43-kDa TAR DNA-binding protein (TDP-43), was recently identified as a component of the ubiquitinated inclusions (UIs) in frontotemporal lobar degeneration (FTLD-U) and sporadic amyotrophic lateral sclerosis (SALS). In the present study using immunohistochemistry, we examined various regions of the nervous system in a series of 35 SALS cases using a polyclonal antibody against TDP-43. Seven of the 35 cases had disease durations of more than 10 years with artificial respiratory support (ARS; duration: 69–156 months). In all cases, TDP-43-immunoreactive (ir) neuronal and glial cytoplasmic inclusions (NCIs and GCIs) were found together in many regions, including the histologically affected lower motor neuron nuclei. Cluster analysis of the distribution pattern of TDP-43-ir NCIs for cases without ARS (n = 28) identified two types (type 1, n = 16; type 2, n = 12). Type 2 was distinguished from type 1 by the presence of TDP-43-ir NCIs in the frontotemporal cortex, hippocampal formation, neostriatum and substantia nigra, and was significantly associated with dementia. Eleven of the 28 cases showed UIs in the hippocampal dentate granule cells, all of which had type-2 distribution pattern. Cases with ARS (n = 7) were also classified into the same types (type 1, n = 5; type 2, n = 2). Cases having type-1 distribution pattern (n = 21) showed no evident neuronal loss in most of the non-motor neuron nuclei where TDP-43-ir NCIs were present, whereas cases having type-2 distribution pattern (n = 14) often showed evident neuronal loss in the frontotemporal cortices, amygdaloid nuclei and substantia nigra. These findings indicate that SALS is a multisystem degenerative disease widely affecting both neurons and glial cells with a heterogeneous pattern of TDP-43-ir NCI distribution (SALS showing type-2 distribution pattern being closely linked to FTLD-U), and that long-term survival supported by a respirator has no apparent influence on the TDP-43 neuronal distribution pattern.
Similar content being viewed by others
Introduction
Amyotrophic lateral sclerosis (ALS) is a fatal neurodegenerative disease of unknown cause in adults. Death caused by respiratory failure comes to most patients within a few years. Most of the cases are sporadic (sporadic ALS: SALS), but 5–10% are familial (familial ALS: FALS) [29]. It is noteworthy that about 20% of FALS cases are reportedly caused by mutations in the Cu/Zn superoxide dismutase (SOD1) gene [8].
Progressive degeneration of both the lower and the upper motor neuron systems is the principal, essential pathological feature of ALS. However, in SALS, there is accumulating evidence that the neurodegenerative process is also present in the non-motor neuron system, including the limbic system, basal ganglia, brainstem and intermediate zone of the spinal cord [11, 21, 25, 37]. In addition, more widespread, severe degeneration has been described in SALS patients who have been on a respirator for a long period [9, 13, 28, 49]. Considering the cellular pathology of SALS, it is of great importance that two characteristic cytoplasmic inclusions—Bunina bodies (BBs) [35, 37] and ubiquitinated skein-like or round inclusions (UIs) [19, 20, 22]—have been described in the histologically affected lower motor neurons. UIs have also been described in neurons in the frontotemporal cortices, including the hippocampal dentate gyrus [14, 15, 34, 36, 46, 47], as well as in those of the neostriatum [16, 37, 45] and the substantia nigra [1, 24, 40] in SALS patients, often with dementia (ALS-dementia) [10, 27, 30].
Recently, a nuclear protein, 43-kDa TAR DNA-binding protein (TDP-43), has been identified as the major pathological protein in sporadic and familial frontotemporal lobar degeneration with UIs (FTLD-U) and in SALS [2, 33]. Subsequently, TDP-43 pathology has been extensively investigated in sporadic and familial FTLD-U [18]. However, the number of studies on ALS appears to be still limited [3, 5, 6, 23, 43, 51]. It is noteworthy that neuronal UIs observed in FALS with SOD1 gene mutation are immunonegative for this protein [23, 43]. With regard to SALS, systemic investigations on the distribution of TDP-43 lesions have not yet been reported.
In a previous study, we confirmed the co-localization of TDP-43 and ubiquitin in UIs, along with a lack of TDP-43 immunoreactivity in cystatin C-immunoreactive (ir) BBs, in the affected lower motor neurons of three patients with SALS [43]. Moreover, TDP-43-ir neuronal and glial cytoplasmic inclusions (NCIs and GCIs) were also observed in several brain regions beyond the affected lower motor neuron nuclei where no UIs were evident, suggesting that SALS may be a multisystem neuro-glial proteinopathy of TDP-43 affecting widely both neurons and glial cells in the central nervous system [43].
In the present study, we performed a more detailed immunohistochemical examination of the distribution of TDP-43-ir NCIs and GCIs, as well as the degenerative lesions (gliosis only, or neuronal loss with gliosis) in the nervous system in a larger series of autopsy cases of SALS.
Materials and methods
Subjects
Brain and spinal cords, as well as peripheral ganglia from 35 patients with sporadic, autopsy-proven ALS were used in the present study. None of the cases were associated with any family history of genetic disorders, or pathological features suggestive of complications arising from other neurodegenerative diseases, including Alzheimer’s disease (AD) and Parkinson’s disease. Among the 35 SALS cases, groups without and with artificial respiratory support (ARS) were recognized, the former (n = 28; cases 1–28) being seen at our department between 1995 and 2005, and the latter (n = 7; cases 29–35) being selected from our departmental autopsy ledger (1962∼), in which the disease durations were more than 10 years (ARS duration: 69–156 months).
The UIs in the hippocampal dentate granule cells (UDG) appear to be a representative lesion in ALS-dementia. To study the association of the occurrence with TDP-43 pathology, cases belonging to these two groups were further divided into two subgroups, without UDG and with UDG, respectively: in the former, 17 cases (cases 1–17) and 11 cases (cases 18–28) belonged to the without-UDG and with-UDG subgroups, respectively, and in the latter, 4 cases (cases 29–32) and 3 cases (cases 33–35) belonged to the without-UDG and with-UDG subgroups, respectively.
Mild-to-moderate dementia was noted in six patients. The presence or absence of dementia was examined by the revised version of the Hasegawa Dementia Rating Scale (HDS-R: a mental examination method commonly used in Japan that utilizes a scale of 0 to 30, where < 21 represents dementia). It has been reported that the HDS-R is better than the Mini-Mental Status Examination (MMSE) as a screening instrument for AD [17]. The clinical findings in the four subgroups among the 35 cases are summarized in Table 1.
Immunohistochemistry
For the present study, we prepared 4-μm-thick, paraffin-embedded sections from the original blocks of various brain and spinal cord regions, as well as from those of the dorsal root (cervical and/or lumbar) and sympathetic (paravertebral and/or celiac) ganglia. These sections were immunostained by the avidin-biotin-peroxidase complex (ABC) method with a Vectastain ABC kit (Vector, Burlingame, CA, USA), using a rabbit polyclonal antibody against TDP-43 (10782-1-AP; Protein Tech Group Inc., Chicago, IL, USA; 1:4,000) [2, 33, 43]. Diaminobenzidine (DAB) was used as the chromogen.
In addition, to assess the association of TDP-43-ir NCIs and GCIs with ubiquitin, a double-labeling immunofluorescence study was performed on several selected regions, using a rabbit polyclonal antibody against TDP-43 (10782-1-AP; Protein Tech Group Inc.; 1:4,000) and mouse monoclonal antibody against ubiquitin (Dako, Glostrup, Denmark; 1:8,000). The second antibodies used were Alexa Fluor 568 goat anti-rabbit IgG (Molecular Probes, Eugene, OR, USA; 1:1000) and Alexa Fluor 488 goat anti-mouse IgG (Molecular Probes; 1:1,000).
Electron microscopy
To observe the ultrastructural profiles of the TDP-43-ir NCIs and GCIs, selected sections immunostained with the anti-TDP-43 antibody were recycled for conventional electron microscopy [38].
Analytical estimation of TDP-43-ir NCI distribution pattern
In each case, TDP-43-ir NCIs in various regions of the nervous system were recorded as absent (0) and present (1). In the present study, the number of neurons having NCIs in each region was not taken into consideration; when observed in individual regions, it was generally much larger in the anterior horns, frontotemporal cortices and amygdaloid nuclei than in the other regions (<10 per region).
A data set of pathological findings for TDP-43-ir NCIs, each coded as “0” or “1”, was obtained from 28 cases without ARS. For factor analysis, we first selected the factors for which data were available for at least 23 cases, and NCIs were detected in at least 4 cases. Missing values were substituted by average values. Statistical analysis was performed using SPSS for Windows (version 12.0.1). From the results of scree plots, we determined the number of factors. We then performed factor analysis (principal factor method) with “Promax’ rotation with Kaiser normalization on these components using the regions with TDP-43-ir NCIs as variables. A factor loading greater than or equal to 0.4 was considered as a cut-off point for interpretation of the factors. By using factor scores from these factors, a Ward’s method, hierarchical cluster analysis using squared Euclidean distance measures, was performed to investigate how the cases were classified into subgroups dependent on the distribution of TDP-43-ir NCIs. Cluster analysis was also performed with the same factors using a data set obtained from all of the 35 cases, including 7 cases with ARS.
Statistical analysis
Comparison of results among the subgroups was performed by the chi-squared (χ2) test using StatView (Abacus Concept, Berkeley, CA, USA). The level of statistical significance was set at P < 0.05.
Pathological evaluation
In all cases, neuronal loss and gliosis were assessed in various regions of the nervous system using hematoxylin-eosin- and Klüver-Barrera-stained sections. When necessary, gliosis was also evaluated using GFAP immunohistochemistry. Neuronal loss in each region was recorded as absent, mild, moderate, or severe, as performed in a previous study [51]. Regions showing only mild gliosis without obvious neuronal loss were also noted.
Results
Distribution of TDP-43-ir NCIs and GCIs
The data obtained from the SALS patients without ARS revealed that TDP-43-ir NCIs and GCIs were present in regions beyond the affected lower motor neuron nuclei (Table 2). In the spinal cord, TDP-43-ir NCIs were found in the anterior horns in almost all cases (Fig. 1a). In the brainstem, they were often found in the red nucleus (Fig. 1b), motor nucleus of the facial nerve, hypoglossal nucleus, reticular formation (Fig. 1c), nucleus ambiguus, and inferior olivary nucleus (Fig. 1d). In the cerebrum, they were often found in the thalamus (Fig. 1e) and the motor cortex (Fig. 1f, g). Although much less frequently, TDP-43-ir NCIs were also found in other regions, including the dorsal root ganglia (Fig. 1h), spinal posterior horn (Fig. 1i), cerebellar dentate nucleus (Fig. 1j), pontine nuclei (Fig. 1k), and oculomotor nucleus (Fig. 1l).
TDP-43 immunostaining revealed neuronal and glial cytoplasmic inclusions (NCIs and GCIs) in many regions of the nervous system in patients with sporadic amyotrophic lateral sclerosis (SALS). TDP-43-immunoreactive (ir) cytoplasmic inclusions are evident in neurons in the lumbar anterior horn (a), red nucleus (b), medulla oblongata reticular formation (c), inferior olivary nucleus (d), thalamus (e), motor cortex [medium-sized pyramidal neuron (f); Betz cell (g)], lumbar dorsal root ganglia (h), lumbar posterior horn (i), cerebellar dentate nucleus (j), pontine nuclei (k), oculomotor nucleus (l), dentate gyrus (granule cells) (m), anterior cingulate cortex (II layer) (n), middle temporal cortex (o), Ammon’s horn (p), amygdaloid nuclei (q), putamen [small neuron (r); large neuron (s)], globus pallidus (internal segment) (t), substantia nigra (u), anterior olfactory nucleus (v) and subthalamic nucleus (w), as well as in glial cells in the lumbar anterior horn (x) and medulla oblongata reticular formation (y). Scale bars = 20 μm
There was a significant difference in the regional frequency of occurrence of TDP-43-ir NCIs between the subgroups with and without UDG (Fig. 1m): they were more frequent in the frontal (Fig. 1n), insular and temporal cortices (Fig. 1o), Ammon’s horn (Fig. 1p), amygdaloid nuclei (Fig. 1q), caudate nucleus, putamen (Fig. 1r, s), globus pallidus (Fig. 1t), superior colliculus, periaqueductal gray, substantia nigra (Fig. 1u), and olfactory bulb (anterior olfactory nucleus) (Fig. 1v) in the former than in the latter (Table 2). Although only a very small number of cases were studied, TDP-43-ir NCIs were also observed in the subthalamic nucleus (Fig. 1w) in the with-UDG subgroup. In this connection, occasional TDP-43-ir dystrophic neurites, together with TDP-43-ir NCIs, were also encountered in the temporal cortices and neostriatum in a proportion of cases.
TDP-43-ir GCIs were also distributed widely in the brain and the spinal cord regions. They were often found in the lower (Fig. 1x) and the upper motor neuron systems, as well as in the brainstem reticular formation (Fig. 1y), and the inferior olivary and amygdaloid nuclei. In several regions, TDP-43-ir GCIs were found more frequently in the with-UDG subgroup than in the without-UDG subgroup (Table 2). No TDP-43-ir intranuclear inclusions were noted in neurons or glial cells in any cases, indicating that intranuclear inclusions are not a feature of SALS.
The data obtained from the SALS patients with ARS were very similar to those of the SALS patients without ARS.
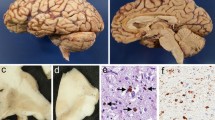
Morphology of TDP-43-ir NCIs and GCIs
As described previously [5, 6, 23, 33, 43], TDP-43-ir NCIs vary in shape, showing a filamentous skein-like, round (often dense-body-like), or somewhat granular appearance (Fig. 1a–w). TDP-43-ir GCIs appeared to occur in oligodendrocytes (Fig. 1y) and also extremely rarely in the radiating processes of astrocytes (Fig. 1x). Ultrastructurally, both the TDP-43-ir NCIs and the GCIs were composed mainly of granulo-filamentous structures (Fig. 2a–d).
Electron microscopy revealed that TDP-43-ir NCIs and GCIs were composed mainly of granulo-filamentous structures. Electron micrographs of sections through Betz cell (a), substantia nigra neuron (b), lumbar anterior horn glial cell (c) and medulla oblongata reticular formation glial cell (d) seen in Fig. 1 g, u, x and y, respectively. Note the coexistence of TDP-43-ir bundles of abnormal filaments, so-called skein-like inclusions in the substantia nigra neuron (b) and medulla oblongata reticular formation glial cell (d). Bundles of glial filaments are evident in the lumbar anterior horn glial cell (astrocyte) (c). Bars a–d 1 μm. Insets: Bars a, b 5 μm; c, d; 2 μm
Association of TDP-43 with ubiquitin
In a previous study, we reported that in SALS, TDP-43-ir NCIs were also found in brain regions where no UIs were observed [43]. It was also noteworthy that ubiquitin immunostaining revealed no immunoreactive structures reminiscent of TDP-43-ir GCIs [43]. In the present study, double-labeling immunofluorescence confirmed co-localization of TDP-43 and ubiquitin in skein-like or round inclusions in the lower motor neurons (Fig. 3a–c), and round or crescent-shaped inclusions in the hippocampal dentate granule cells and neostriatal small neurons. However, double-labeling immunofluorescence revealed that TDP-43-ir NCIs in the non-motor neuron nuclei, such as the globus pallidus and thalamus (Fig. 3d–f, g–i), and motor cortex, as well as GCIs in the gray (Fig. 3j–l) and white matter, were only weakly, or not ubiquitinated.
Double-labeling immunofluorescence with the polyclonal anti-TDP-43 and monoclonal anti-ubiquitin antibodies. Co-localization of TDP-43 with ubiquitin is evident in cytoplasmic inclusions in a cervical anterior horn cell (a–c). However, weak or absent co-localization of TDP-43 with ubiquitin is shown in cytoplasmic inclusions in a globus pallidus (internal segment) neuron (d–f), as well as in a thalamus neuron (g–i). Weak or absent ubiquitin immunoreactivity in TDP-43-ir cytoplasmic inclusions is also shown in a motor cortex glial cell (j–l). a, d, g, j TDP-43; b, e, h, k ubiquitin, c, f, i, l merged. Bars 20 μm
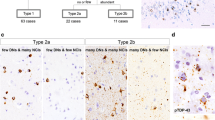
Classification of SALS based on distribution pattern of TDP-43-ir NCIs
We performed cluster analysis of TDP-43-ir NCI distribution in SALS cases without ARS. Factor analysis of the regions with TDP-43-ir NCIs identified two levels of attribution, frontotemporal cortex-hippocampal formation-neostriatum-substantia nigra and motor cortex-midbrain non-motor neuron nuclei (except the substantia nigra) (Table 3). Cluster analysis of the two factor scores identified two types (types 1 and 2) among the 28 SALS cases without ARS (Fig. 4). Type 2 was distinguished from type 1 by the presence of TDP-43-ir NCIs in the frontotemporal cortex, hippocampal formation, neostriatum and substantia nigra. All of the 11 SALS cases belonging to the without-ARS/with-UDG subgroup were subclassified into type 2 (Fig. 4).
Cluster analysis and distribution of TDP-43-ir NCIs in SALS. Upper panel Dendrogram of cluster analysis of the distribution of TDP-43-ir NCIs in SALS cases without ARS (left 28 cases). Black numbers indicate the SALS case numbers without ubiquitinated inclusions in the hippocampal dentate granule cells (UDG) and red numbers indicate the SALS case numbers with UDG. Lower panel Distribution of TDP-43-ir NCIs in SALS cases without ARS (left 28 cases) and with ARS (right 7 cases). Factors that were used in cluster analysis are shown in red (factor 1: frontotemporal cortex-hippocampal formation-neostriatum-substantia nigra) and blue (factor 2: motor cortex-midbrain non-motor neuron nuclei)
In the 28 cases without ARS, the clinical features were compared between the two types of TDP-43 neuronal distribution pattern. There was no significant difference in the age at onset or the disease duration between the two types. Dementia was consistently associated with type-2 distribution pattern (Table 4); qualitatively, no obvious correlation was noted between the severity of frontotemporal cortical pathology and that of dementia.
Next, we investigated the pattern of distribution of TDP-43-ir NCIs in the SALS cases with ARS. The distribution patterns of TDP-43-ir NCIs in these cases appeared to be essentially the same as those in cases without ARS (Fig. 4). Cluster analysis of the two factor scores for all the 35 SALS cases with or without ARS also identified two types (types 1 and 2), and the 7 SALS cases with ARS were also classified into two types that were identical to types 1 and 2 detected among the 28 SALS without ARS (data not shown), indicating that there was no significant difference in the distribution pattern of TDP-43-ir NCIs between the subgroups with and without ARS.
Retrospectively, the number of neurons having TDP-43-ir NCIs in each region was in general larger in cases with type-2 distribution pattern than in those with type-1distribution pattern.
Neuronal loss and gliosis
The severity of neuronal loss in various regions of the nervous system is shown in Fig. 5. Neuronal loss was evident in the lower and upper motor neuron systems (except lower motor neuron nuclei innervating to the extraocular muscles) in all cases. Generally, the degree of neuronal loss in the motor cortex appeared to be well correlated with that of myelin pallor in the corticospinal tracts (including the pyramides). In cases showing type-1 distribution pattern, neuronal loss was not evident in most of the non-motor neuron nuclei. However, in cases showing type-2 distribution pattern, neuronal loss was also evident in the frontotemporal cortices, amygdaloid nuclei and substantia nigra. Types 1 and 2 TDP-43 neuronal distribution pattern are illustrated schematically in Fig. 6, which also shows the data for both TDP-43 NCI regional frequency and regional severity of neuronal loss.
Distribution and severity of neuronal loss in the 35 SALS cases studied. It is apparent that widespread degenerative changes are a feature in type-2 TDP-43 neuronal distribution pattern in both the without-ARS and with-ARS subgroups. Such changes appear to be more marked in the with-ARS/with-UDG subgroup than in the without-ARS/with-UDG subgroup
Schematic illustration of the two types of neuronal pathological TDP-43 distribution pattern. Regional frequency of the inclusions and regional severity of neuronal loss are also shown. Type 1 appears to represent the TDP-43 distribution pattern observed in cases of so-called classical SALS. Type 2 appears to represent the TDP-43 distribution pattern observed in cases of ALS-dementia (regardless of the clinical presence or the absence of dementia)
Discussion
In the present study, the occurrence of both TDP-43-ir NCIs and GCIs was confirmed in the affected lower motor neuron nuclei. In addition, in some cases, the lower motor neurons innervating the extraocular muscles, as well as the upper motor neurons, so-called Betz cells, in the motor cortex were also found to be affected by TDP-43 pathology. These findings provided the first molecular evidence that in SALS, both lower and upper motor neurons are widely involved in the common pathological process involving TDP-43 metabolic abnormality. Moreover, TDP-43-ir NCIs and GCIs were also observed in regions beyond the lower and upper motor neuron systems. Interestingly, TDP-43-ir NCIs were found occasionally in the anterior olfactory nucleus and dorsal root ganglia. Ubiquitin pathology has already suggested that SALS is a multisystem neurological disease [11, 21, 25, 37]. However, in the present study, TDP-43 pathology showed more widespread lesions affecting both neurons and glial cells in the nervous system. If TDP-43 is regarded as the major disease protein [2, 33], SALS must be a multisystem neuro-glial proteinopathy of TDP-43.
In addition, we demonstrated the presence of two types of SALS pathology based on the distribution patterns of TDP-43-ir NCIs and found that the presence of UDG was a good predictor of the type-2 distribution pattern that was significantly associated with dementia. Okamoto et al. [34] first reported that UIs can also occur in the hippocampal dentate granule cells in patients with SALS. This was later shown to be a feature of ALS-dementia [14, 15, 36, 46, 47], which is now widely recognized as FTLD with motor neuron disease (MND) [4, 26, 31]. We showed that the SALS cases with UDG were subclassifiable into a distinct subgroup showing type-2 distribution pattern, based on the distribution pattern of TDP-43-ir NCIs, indicating the existence of a particular pathological variant of SALS.
Does long-term survival with respiratory assistance have an effect on the neuropathological findings in SALS patients? It has been reported that the ultimate manifestation of SALS is a totally locked-in state with widespread degeneration (severe neuronal loss and gliosis), including the motor neuron system [9, 13, 28]. It has also been reported that such lesions are not always a feature in SALS patients that have survived for long period with respiratory assistance [13, 37, 50]. In the present study, it became apparent that there was no significant difference in the distribution pattern of TDP-43-ir NCIs between the subgroups with and without ARS. On the other hand, there appeared to be some expansion of degenerative lesion distribution in the seven cases with ARS; it was noteworthy that in the two cases showing type-2 distribution pattern, there was evident neuronal loss in many brain regions. Based on these findings, it may be possible to consider that the type-2 distribution pattern predisposes SALS patients to a totally locked-in state with widespread degeneration during long-term survival on respirators [9, 13, 28, 49]. In other words, SALS patients having type-1 distribution pattern may hardly develop such changes even during long-term survival on respirators, and dementia may not be a feature in these patients, in accord with previous clinicopathological observations [13, 37, 50].
Is the abnormal cytoplasmic aggregation of TDP-43 actually associated with neuronal cell death? In relation to SALS, it may be permissible to discuss this important issue to a certain degree based on the results obtained in the present study, although no quantitative measurements were used in the assessment of TDP-43 pathology and neuronal loss. Indeed, the regions where TDP-43-ir NCIs were present mostly overlapped the regions where degenerative changes were evident. However, the issue of cell death may not be so straightforward. Although neuronal loss was observed in the motor cortex in all cases, TDP-43-ir NCIs were present in less than 50% (15/35) of cases, and TDP-43-ir GCIs were present in 80% (28/35), not 100%, of cases (data not shown). Furthermore, not all non-motor neurons possessing TDP-43-ir NCIs were lost; particularly, the presence of ubiquitin- and TDP-43-ir NCIs in the hippocampal dentate granule cells was considered to be a characteristic feature of type-2 distribution pattern, whereas granule cell loss was not a feature. It was also of interest that TDP-43-ir NCIs observed in some non-motor neuron nuclei were only weakly, or not ubiquitinated, suggesting that there was a lack of aggressive participation of ubiquitin in the proteolytic pathway for degradation of TDP-43 cytoplasmic aggregates in these inclusion-bearing neurons. This was also the case for TDP-43-ir GCIs observed in the gray and white matter. Similar observations have been reported in cases of FTLD-U [32] and FTLD with MND [3].
Moreover, we have investigated morphometrically the presence or the absence of neuronal loss in the spinal Clarke’s column and intermediolateral nucleus in SALS patients with and without ARS, and found that in these regions, neurons tended to disappear with time after the start of ARS [41, 42], suggesting that these sensory or autonomic neurons and anterior horn cells differ in their rate of degeneration. In the present study, neuronal loss and gliosis were confirmed in these spinal cord non-motor neuron nuclei in many cases with ARS. However, no TDP-43-ir NCIs or GCIs could be detected there in any of the cases studied.
In conclusion, we have demonstrated widespread occurrence of TDP-43-ir NCIs and GCIs in the nervous system of patients with SALS. The distribution pattern of TDP-43-ir NCIs could be subclassified into two types (types 1 and 2); type-2 distribution pattern, which was highly predictable by detection of UDG, was significantly associated with dementia (SALS showing type-2 distribution pattern being closely linked to FTLD-U [4, 26]). Recently, TDP-43-ir NCI distribution pattern very similar, if not identical, to the type 2 has been clearly demonstrated in two cases of sporadic FTLD with MND [3]. The two types of TDP-43 neuronal distribution pattern were not influenced by long-term survival with respiratory support, suggesting that the two TDP-43 subgroups may represent distinctly different pathogenic processes. Finally, whether or not there is a distinct correlation between TDP-43 distribution pattern and cell death awaits further detailed molecular and genetic studies. At present, it is of great interest that mutations in TDP-43 gene have been identified in rapid succession in several FALS and SALS cases [7, 12, 39, 44, 48].
References
Al-Sarraj S, Maekawa S, Kibble M, Everall I, Leigh N (2002) Ubiquitin-only intraneuronal inclusion in the substantia nigra is a characteristic feature of motor neuron disease with dementia. Neuropathol Appl Neurobiol 28:120–128
Arai A, Hasegawa M, Akiyama H, Ikeda K, Nonaka T, Mori H, Mann D, Tsuchiya K, Yoshida M, Hashizume Y, Oda T (2006) TDP-43 is a component of ubiquitin-positive inclusions in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Biochem Biophys Res Commun 351:602–611
Brandmeir NJ, Geser F, Kwong LK, Zimmerman E, Qian J, Lee VM-Y, Trojanowski JQ (2008) Severe subcortical TDP-43 pathology in sporadic frontotemporal lobar degeneration with motor neuron disease. Acta Neuropathol 115:123–131
Cairns NJ, Bigio EH, Mackenzie IR, Neumann M, Lee VM-Y, Hatanpaa KJ, White III CL, Schneider JA, Grinberg LT, Halliday G, Duyckaerts C, Lowe JM, Holm IE, Tolnay M, Okamoto K, Yokoo H, Murayama S, Woulfe J, Munoz DG, Dickson DW, Ince P, Trojanowski JQ, Mann DM (2007) Neuropathologic diagnostic and nosologic criteria for frontotemporal lobar degeneration: consensus of the Consortium for Frontotemporal Lobar Degeneration. Acta Neuropathol 114:5–22
Davidson Y, Kelley T, Mackenzie IR, Pickering-Brown S, Plessis DD, Neary D, Snowden JS, Mann DM (2007) Ubiquitinated pathological lesions in frontotemporal lobar degeneration contain the TAR DNA-binding protein, TDP-43. Acta Neuropathol 113:521–533
Dickson DW, Josephs KA, Amador-Ortiz (2007) TDP-43 in differential diagnosis of motor neuron disorders. Acta Neuropathol 114:39–47
Gitcho MA, Baloh RH, Chakraverty S, Mayo K, Norton JB, Levitch D, Hatanpaa KJ, White CL 3rd, Bigio EH, Caselli R, Baker M, Al-Lozi MT, Morris JC, Pestronk A, Rademakers R, Goate AM, Cairns NJ (2008) TDP-43 A315T mutation in familial motor neuron disease. Ann Neurol 63:535–538
Gros-Louis F, Gaspar C, Rouleau GA (2006) Genetics of familial and sporadic amyotrophic lateral sclerosis. Biochim Biophys Acta 1762:956–972
Hayashi H, Kato S (1989) Total manifestation of amyotrophic lateral sclerosis. ALS in the totally locked-in state. J Neurol Sci 93:19–35
Hudson AJ (1981) Amyotrophic lateral sclerosis and its association with dementia, parkinsonism and other neurological disorders: a review. Brain 104:217–247
Ince PG, Lowe J, Shaw PJ (1998) Amyotrophic lateral sclerosis: current issues in classification, pathogenesis and molecular pathology. Neuropathol Appl Neurobiol 24:104–117
Kabashi E, Valdmanis PN, Dion P, Spiegelman D, McConkey BJ, Velde CV, Bouchard JP, Lacomblez L, Pochigaeva K, Salachas F, Pradat PF, Camu W, Meininger V, Dupre N, Rouleau GA (2008) TARDBP mutations in individuals with sporadic and familial amyotrophic lateral sclerosis. Nat Genet 40:572–574
Kato S, Hayashi H, Oda M, Kawata A, Shimizu T, Hayashi M, Dugaya K, Arai N (1996) Neuropathology in sporadic ALS patients on respirators. In: Nakano I, Hirano A (eds) Amyotrophic lateral sclerosis: progress and perspectives in basic research and clinical application. Elsevier, Amsterdam, pp 66–77
Kato S, Oda M, Hayashi H, Kawata A, Shimizu T (1994) Participation of the limbic system and its associated area in the dementia of amyotrophic lateral sclerosis. J Neurol Sci 126:62–69
Kawashima T, Doh-ura K, Kikuchi H, Iwaki T (2001) Cognitive dysfunction in patients with amyotrophic lateral sclerosis is associated with spherical or crescent-shaped ubiquitinated intraneuronal inclusions in the parahippocampal gyrus and amygdala, but not in the neostriatum. Acta Neuropathol 102:467–472
Kawashima T, Kikuchi H, Takita M, Doh-ura K, Ogomori K, Oda M, Iwaki T (1998) Skein-like inclusions in the neostriatum from a case of amyotrophic lateral sclerosis with dementia. Acta Neuropathol 96:541–545
Kim KW, Lee DY, Jhoo JH, Youn JC, Suh YJ, Jun YH, Seo EH, Woo JI (2005) Diagnostic accuracy of minimental status examination and revised Hasegawa dementia scale for Alzheimer’s disease. Dement Geriatr Cogn Disord 19:324–330
Kwong LK, Neumann M, Sampathu DM, Lee V M-Y, Trojanowski JQ (2007) TDP-43 proteinopathy: the neuropathology underlying major forms of sporadic and familial frontotemporal degeneration and motor neuron disease. Acta Neuropathol 114:63–70
Leigh PN, Anderton BH, Dodson A, Gallo JM, Swash M, Power DM (1988) Ubiquitin deposits in anterior horn cells in motor neuron disease. Neurosci Lett 93:197–203
Leigh PN, Withwell H, Garofalo O, Buller J, Swash M, Martin JE, Gallo JM, Weller RO, Anderton BH (1991) Ubiquitin-immunoreactive intraneuronal inclusions in amyotrophic lateral sclerosis. Morphology, distribution, and specificity. Brain 114:775–788
Lowe J (1994) New pathological findings in amyotrophic lateral sclerosis. J Neurol Sci 124(Suppl):38–51
Lowe J, Lennox G, Jefferson D, Morrell K, McQuire D, Gray T, Landon M, Doherty FJ, Mayer RJ (1988) A filamentous inclusion body within anterior horn neurons in motor neuron disease defined by immunocytochemical localization of ubiquitin. Neurosci Lett 94:203–210
Mackenzie IR, Bigio EH, Ince PG, Geser F, Neumann M, Cairns NJ, Kwong L, Forman MS, Ravits J, Stewart H, Eisen A, McClusky L, Kretzschmar HA, Monoranu CM, Highley JR, Kirby J, Siddique T, Shaw PJ, Lee VM-Y, Trojanowski JQ (2007) Pathological TDP-43 distinguishes sporadic amyotrophic lateral sclerosis from amyotrophic lateral sclerosis with SOD1mutations. Ann Neurol 61:427–434
Mackenzie IR, Feldman H (2004) Extrapyramidal features in patients with motor neuron disease and dementia; a clinicopathological correlative study. Acta Neuropathol 107:336–340
Mackenzie IR, Feldman HH (2005) Ubiquitin immunohistochemistry suggest classic motor neuron disease, motor neuron disease with dementia, and frontotemporal dementia of motor neuron disease type represent a clinicopathologic spectrum. J Neuropathol Exp Neurol 64:730–739
McKhann GM, Albert MS, Grossman M, Miller B, Dickson D, Trojanowski JQ Work Group on Frontotemporal Dementia, Pick’s disease (2001) Clinical and pathological diagnosis of frontotemporal dementia: report of the work group of frontotemporal demetia and Pick’s disease. Arch Neurol 58:1803–1809
Mitsuyama Y (1984) Presenile dementia with motor neuron disease in Japan: clinicopathological review of 26 cases. J Neurol Neurosurg Psychiatry 47:953–959
Mizutani T, Sakamaki S, Tsuchiya N, Namei S, Kohzu H, Horiuchi R, Ida M, Shiozawa R, Takasu T (1992) Amyotrophic lateral sclerosis with ophthalmoplegia and multisystem degeneration in patients on long-term use of respitators. Acta Neuropathol 84:372–377
Mulder DW, Kurland LT, Offord KP, Beard CM (1986) Familial adult motor neuron disease: amyotrophic lateral sclerosis. Neurology 36:511–517
Nakano I (1993) Temporal lobe lesions in amyotrophic lateral sclerosis with or without dementia: a neuropathological study. Neuropathology 13:215–227
Nakano I (2000) Frontotemporal dementia with motor neuron disease (amyotrophic lateral sclerosis with dementia). Neuropathology 20:68–75
Neumann M, Kwong LK, Truax AC, Vanmassenhove B, Kretzschmar HA, Van Deerlin VM, Clark CM, Grossman M, Miller BL, Trojanowski JQ, Lee VM-Y (2007) TDP-43-positive white matter pathology in frontotemporal lobar degeneration with ubiquitin-positive inclusions. J Neuropathol Exp Neurol 66:177–183
Neumann M, Sampathu DM, Kwong LK, Truax AC, Micsenyi MC, Chou TT, Bruce J, Schuck T, Grossman M, Clark CM, McCluskey LF, Miller BK, Masliah E, Mackenzie IR, Feldman H, Feiden W, Kretzschmar HA, Trojanowski JQ, Lee VM-Y (2006) Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science 314:130–133
Okamoto K, Hirai S, Yamazaki T, Sun XY, Nakazato Y (1991) New ubiquitin-positive intraneuronal inclusions in the extra-motor cortices in patients with amyotrophic lateral sclerosis. Neurosci Lett 129:233–236
Okamoto K, Mizuno Y, Fujita Y (2008) Bunina bodies in amyotrophic lateral sclerosis. Neuropathology 28:109–115
Okamoto K, Murakami N, Kusaka H, Yoshida M, Hashizume Y, Nakazato Y, Matsubara E, Hirai S (1992) Ubiquitin-positive intraneuronal inclusions in the extramotor cortices of presenile dementia patients with motor neuron disease. J Neurol 239:426–430
Piao Y-S, Wakabayashi K, Kakita A, Yamada M, Hayashi S, Morita T, Ikuta F, Oyanagi K, Takahashi H (2003) Neuropathology with clinical correlations of sporadic amyotrophic lateral sclerosis: 102 autopsy cases examined between 1962 and 2000. Brain Pathol 13:10–22
Rossi GL, Luginbühl H, Probst D (1970) A method for ultrastructural study of lesions found in conventional histological sections. Virchows Arch [A] 350:216–224
Sreedharan J, Blair IP, Tripathi VB, Hu X, Vance C, Rogelj B, Ackerley S, Durnall JC, Williams KL, Buratti E, Baralle F, de Belleroche J, Mitchell JD, Leigh PN, Al-Chalabi A, Miller CC, Nicholson G, Shaw CE (2008) TDP-43 mutations in familial and sporadic amyotrophic lateral sclerosis. Science 319:1668–1672
Su M, Yoshida Y, Ishiguro H, Hirota K (1999) Nigral degeneration in a case of amyotrophic lateral sclerosis: evidence of Lewy body-like and skein-like inclusions in the pigmented neurons. Clin Neuropathol 18:293–300
Takahashi H, Oyanagi K, Ikuta F (1993) The intermediolateral nucleus in sporadic amyotrophic lateral sclerosis. Acta Neuropathol 86:190–192
Takahashi H, Oyanagi K, Ohama E, Ikuta F (1992) Clarke’s column in sporadic amyotrophic lateral sclerosis. Acta Neuropathol 84:465–470
Tan C-F, Eguchi H, Tagawa A, Onodera O, Iwasaki T, Tsujino A, Nishizawa M, Kakita A, Takahashi H (2007) TDP-43 immunoreactivity in neuronal inclusions in familial amyotrophic lateral sclerosis with or without SOD1 gene mutation. Acta Neuropathol 113:535–542
Van Deerlin VM, Leverenz JB, Bekris LM, Bird TD, Yuan W, Elman LB, Clay D, Wood EM, Chen-Plotkin AS, Martinez-Lage M, Steinbart E, McCluskey L, Grossman M, Neumann M, Wu IL, Yang WS, Kalb R, Galasko DR, Montine TJ, Trojanowski JQ, Lee VM, Schellenberg GD, Yu CE (2008) TARDBP mutation in amyotrophic lateral sclerosis with TDP-43 neuropathology: a genetic and histopathological analysis. Lancet Neurol 7:409–416
Wakabayashi K, Piao Y-S, Hayashi S, Kakita A, Yamada M, Takahashi H (2001) Ubiquitinated neuronal inclusions in the neostriatum in patients with amyotrophic lateral sclerosis with and without dementia—a study of 60 patients 31 to 87 years of age. Clin Neuropathol 20:47–52
Wightman G, Anderson VER, Martin J, Swash M, Anderton BH, Neary D, Mann D, Luthert P, Leigh PN (1992) Hippocampal and neocortical ubiquitin-immunoreactive inclusions in amyotrophic lateral sclerosis with dementia. Neurosci Lett 139:269–274
Wilson CM, Grace GM, Munoz DG, He BP, Strong MJ (2001) Cognitive impairment in sporadic ALS. A pathologic continuum underlying a multisystem disorder. Neurology 57:651–657
Yokoseki A, Shiga A, Tan C-F, Tagawa A, Kaneko H, Koyama A, Eguchi H, Tsujino A, Ikeuchi T, Kakita A, Okamototo K, Nishizawa M, Takahashi H, Onodera O (2008) TDP-43 mutation in familial amyotrophic lateral sclerosis. Ann Neurol 63:538–542
Yoshida M (2004) Amyotrophic lateral sclerosis with dementia: the clinicopathological spectrum. Neuropathology 24:87–102
Yoshida M, Murakami N, Hashizume Y, Itoh E, Takahashi A (1992) A clinicopathological study of two respirator-aided long-survival cases of amyotrophic lateral sclerosis (in Japanese with English abstract). Rinsho Shikeigaku 32:259–265
Zhang H, Tan C-F, Mori F, Tanji K, Kakita A, Takahashi H, Wakabayashi K (2008) TDP-43-immunoreactive neuronal and glial inclusions in the neostriatum in amyotrophic lateral sclerosis with and without dementia. Acta Neuropathol 115:115–122
Acknowledgments
We thank C. Tanda, J. Takasaki, N. Kaneko, Y. Ota and S. Egawa for their technical assistance, and M. Machida for her help in preparing the manuscript. This work was supported by a grant from the Research Committee on Neurodegenerative Diseases, Ministry of Health, Labor and Welfare, and a grant-in-Aid for Scientific Research on Priority Areas “Advanced Brain Science Project” and “Applied Genomics” from the Ministry of Education, Science, Sports and Culture, Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nishihira, Y., Tan, CF., Onodera, O. et al. Sporadic amyotrophic lateral sclerosis: two pathological patterns shown by analysis of distribution of TDP-43-immunoreactive neuronal and glial cytoplasmic inclusions. Acta Neuropathol 116, 169–182 (2008). https://doi.org/10.1007/s00401-008-0385-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-008-0385-z