Abstract
We previously reported HLA allelic associations with vaccinia virus (VACV)-induced adaptive immune responses in a cohort of healthy individuals (n = 1,071 subjects) after a single dose of the licensed smallpox (Dryvax) vaccine. This study demonstrated that specific HLA alleles were significantly associated with VACV-induced neutralizing antibody (NA) titers (HLA-B*13:02, *38:02, *44:03, *48:01, and HLA-DQB1*03:02, *06:04) and cytokine (HLA-DRB1*01:03, *03:01, *10:01, *13:01, *15:01) immune responses. We undertook an independent study of 1,053 healthy individuals and examined associations between HLA alleles and measures of adaptive immunity after a single dose of Dryvax-derived ACAM2000 vaccine to evaluate previously discovered HLA allelic associations from the Dryvax study and determine if these associations are replicated with ACAM2000. Females had significantly higher NA titers than male subjects in both study cohorts [median ID50 discovery cohort 159 (93, 256) vs. 125 (75, 186), p < 0.001; replication cohort 144 (82, 204) vs. 110 (61, 189), p = 0.024]. The association between the DQB1*03:02 allele (median ID50 discovery cohort 152, p = 0.015; replication cohort 134, p = 0.010) and higher NA titers was replicated. Two HLA associations of comparable magnitudes were consistently found between DRB1*04:03 and DRB1*08:01 alleles and IFN-γ ELISPOT responses. The association between the DRB1*15:01 allele with IFN-γ secretion was also replicated (median pg/mL discovery cohort 182, p = 0.052; replication cohort 203, p = 0.014). Our results suggest that smallpox vaccine-induced adaptive immune responses are significantly influenced by HLA gene polymorphisms. These data provide information for functional studies and design of novel candidate smallpox vaccines.
Similar content being viewed by others
Introduction
Vaccinia virus (VACV) continues to be a topic of interest, specifically its use as a viral vaccine to prevent smallpox. VACV is capable of eliciting robust, long-lasting humoral and cellular immune responses against a wide variety of orthopox viruses, including variola virus (smallpox) (Amara et al. 2004; Bhanuprakash et al. 2012). The NYCBH strain of VACV was used to create the first smallpox vaccine in the late nineteenth century after undergoing several passages in heifers. After the eradication of smallpox in 1979 (Henderson 1998), a more modern VACV vaccine, ACAM2000, was created by culturing a Dryvax-derived VACV strain in Vero cells (Osborne et al. 2007) and has since been used in vaccination efforts post-2008. Not only do current VACV-based vaccines have the potential to protect the population against smallpox disease in the event of biological warfare, they could also be used to prevent potential disease caused by the emergence of new infectious orthopox viruses (Verardi et al. 2012; Walsh and Dolin 2011).
Although VACV was effective at eradicating smallpox (along with other public health interventions), it elicits varied immune responses between vaccinated individuals (Henderson 1998; Poland et al. 2007). These inter-individual differences in immune responses to smallpox vaccine are partly explained by the genetic variability between vaccinated individuals, including polymorphisms in human leukocyte antigen (HLA) genes (Poland et al. 2007). The major function of HLA molecules is to present VACV antigens to T cells, thereby initiating adaptive immune responses. Associations between humoral and cellular immune responses and HLA polymorphisms have already been demonstrated for a wide variety of other viral and bacterial vaccines, including measles, mumps, rubella, influenza, hepatitis B, and anthrax although the results of these studies have been varied, in part, due to the population allele frequencies or small numbers of study subjects (Narwaney et al. 2013; Ovsyannikova et al. 2006; Li et al. 2009; Ovsyannikova et al. 2013b; Pajewski et al. 2011). In order to better understand the effectiveness and efficacy of VACV smallpox vaccines within the population, it is necessary to identify the impact of HLA and non-HLA immune-associated gene polymorphisms on adaptive immune responses to smallpox vaccine.
Very few immunogenetic studies have been conducted on smallpox vaccine in regard to potential associations between HLA (de Vries et al. 1977; Ovsyannikova et al. 2011) and non-HLA gene polymorphisms and immune responses to primary smallpox vaccine (Haralambieva et al. 2011; Kennedy et al. 2012; Ovsyannikova et al. 2012a, b, 2013a). Our previous study identified several candidate HLA polymorphisms within a cohort of 1,071 healthy individuals that were associated with varied inter-individual humoral and cellular (cytokine) immune responses to smallpox (Dryvax) vaccine. These alleles included HLA-B (*13:02, *38:02, *44:03, *48:01) and HLA-DQB1 (*03:02, *06:04) when neutralizing antibody titers were used as the humoral immune measure, and HLA-DRB1 (*01:03, *03:01, *10:01, *13:01, *15:01) when IFN-γ ELISPOT assays were used as the cellular immune measure (Ovsyannikova et al. 2011). Although this information is highly valuable, replication studies are essential to validate the results of these findings.
To confirm the results of our initial study, we conducted a study on an independent cohort of 1,053 healthy individuals to examine associations between HLA alleles and measures of both humoral and cellular immune responses to smallpox (ACAM2000) vaccine. The aim of this study was to evaluate the significant associations identified in our earlier Dryvax study and replicate previously discovered associations between specific HLA class I and class II alleles and VACV-induced neutralizing antibody titers and markers of cell-mediated VACV immunity after ACAM2000 vaccination.
Methods
Study subjects
Two cohorts of study subjects, previously described in our earlier work (Haralambieva et al. 2011; Kennedy et al. 2008; Ovsyannikova et al. 2011, 2013a), were also used for the current study (see Table 1). In brief, we enrolled 1,076 healthy armed forces personnel between 18 to 40 years of age during 2005–2006 (San Diego cohort, i.e., discovery cohort). All subjects received a single dose of a US-licensed smallpox [Dryvax, New York City Board of Health (NYCBOH) strain, Wyeth Laboratories] vaccine during the period of 2002–2006. Of these 1,076 subjects, 1,071 met our inclusion and exclusion criteria and were used in this study. Briefly, study subjects were included if they developed a “take” after vaccination and if they were not enrolled in our previous smallpox vaccine immunogenetics study; study subjects were excluded from this study if they failed to develop a “take” after vaccination, were previously unexposed to smallpox, were under the age of 18 years old, or were pregnant, imprisoned, or institutionalized during sample collection.
We enrolled an additional 1,136 healthy subjects, between 19 and 40 years of age during 2010–2011, who were immunized with a single dose of a smallpox vaccine (ACAM2000, NYCBOH strain, Acambis) between 2006 and 2010 (US cohort, i.e., replication cohort). Of these 1,136 subjects, 1,053 provided a blood sample and met the above inclusion and exclusion criteria. The Institutional Review Boards of the Mayo Clinic (Rochester, Minnesota) and Naval Health Research Center (San Diego, California) granted permission for the study, and written informed consent was obtained before enrollment of each subject.
Neutralizing antibody assay
VACV neutralizing antibody assay methods described herein are similar or identical to those published for our previous VACV studies (Kennedy et al. 2009; Ovsyannikova et al. 2011). The neutralizing antibody assay was performed on the discovery cohort (n = 1,071) five years prior to that of replication cohort (n = 1,053); however, antibody measurements were performed using an identical protocol and assay conditions. In brief, antibody titers were measured using an optimized VACV-specific neutralizing antibody assay, using β-galactosidase expressing VACV, as previously described (Kennedy et al. 2009; Manischewitz et al. 2003; Ovsyannikova et al. 2011). Results for each subject are reported as the serum dilution that inhibits 50 % of VACV activity (ID50 titer). Each serum sample was tested in triplicate in the discovery cohort and in five replicates in the replication cohort. The average coefficient of variation for this assay was 6.9 % (Kennedy et al. 2009).
IFN-γ ELISPOT assay
Enzyme-linked immunosorbent spot (ELISPOT) assays (R&D Systems) were performed to measure total peripheral blood mononuclear cell (PBMC) IFN-γ and CD8α+ IFN-γ secretion, as previously reported (Ovsyannikova et al. 2011, 2013a). ELISPOT assays on the discovery cohort (total PBMC IFN-γ ELISPOT, n = 1,058; CD8α+ IFN-γ ELISPOT, n = 1,002) were performed 6 years prior to that of replication cohort (total PBMC IFN-γ ELISPOT, n = 1,048; CD8α+ IFN-γ ELISPOT, n = 991). PBMCs were stimulated for 24 h with inactivated VACV at a multiplicity of infection (MOI) of 5 and an MOI of 1 for the discovery and replication cohorts, respectively. These parameters were set based upon the results of optimization performed prior to each independent study. Outcomes are expressed as spot-forming cells (SFC) per 2 × 105 PBMCs. Plates were scanned, and spots were counted with an ImmunoSpot S4 Pro-Analyzer using ImmunoSpot software, version 4.0 (Cellular Technology). Intraclass correlations ranged between 0.60 (total PBMC IFN-γ ELISPOT) to 0.63 (CD8α+ IFN-γ ELISPOT).
Cytokine measurements
Enzyme-linked immunosorbent assays (ELISAs) were performed in both cohorts, six years apart, to measure cytokine secretion from cell culture supernatants, as previously described (Ovsyannikova et al. 2011, 2012a). In brief, PBMCs were plated at a concentration of 2 × 105 cells per well prior to stimulation with inactivated VACV. Optimal assay parameters for the discovery cohort have been previously described (Ovsyannikova et al. 2011). Conditions for viral stimulation in the replication cohort were optimized and are as follows: for IFN-α (n = 1,039) and IFN-γ (n = 1,039), the MOI was 0.05 (4 days); for IL-12p40 (n = 1,041), TNF-α (n = 1,041), and IL-1β (n = 1,041), the MOI was 0.5 (24 h); for IL-2 (n = 1,026), the MOI was 5 (24 h); and for IL-6 (n = 1,031), the MOI was 5 (8 days). The intraclass correlation coefficients for IFN-α, IFN-γ, IL-12p40, TNF-α, IL-1β, IL-2, and IL-6 measures of smallpox vaccine immunity were 0.42, 0.59, 0.65, 0.50, 0.75, 0.55, and 0.76, respectively.
HLA genotyping
Discovery cohort genotyping was performed by high-resolution PCR-SSP, as previously described (Ovsyannikova et al. 2011). Replication cohort HLA class I (A, B, and C) and class II (DRB1, DQA1, DQB1, DPA1, and DPB1) allele typing was performed using high-throughput, high-fidelity genotyping with deep sequencing technology, which combines the advantage of long-range amplification with the power of high-throughput Illumina sequencing platforms, developed at the Stanford Genome Technology Center (Dr. Michael Mindrinos, Stanford School of Medicine, Palo Alto, CA) (Wang et al. 2012).
Statistical methods
Demographic and immune outcome variables were summarized within cohorts utilizing similar methods to those published in our previous HLA studies (Ovsyannikova et al. 2009, 2011); counts and percentages for categorical variables and medians and 25th and 75th percentiles for quantitative variables. The difference between the median values from the stimulated and unstimulated replicate values was calculated prior to summarizing the immune response outcomes measured from smallpox virus-stimulated and unstimulated cells (ELISA- and ELISPOT-based assays). Chi square and Kruskal–Wallis tests were conducted to investigate differences between cohorts for categorical and quantitative features, respectively. The logarithm of the ID50 was used as the response variable, and Van der Waerden normal scores of the ELISA and ELISPOT outcomes were used as the responses in the analyses to ensure that the data conformed to statistical assumptions.
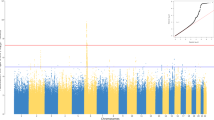
Linear regression models were used to test for HLA associations with the log-transformed ID50 values, and linear mixed effects models were used to test for HLA associations with the inverse normal-transformed results from the other assays. All analyses were performed while adjusting for assay batch, gender, age at blood draw, time from vaccination to blood draw, and the first three eigenvectors from the principal component analysis conducted to quantify fine-scale genetic differences among individuals. The age and time variables were categorized into quartiles prior to analysis. In the linear mixed effects models, all of the repeated stimulated and unstimulated results were included in a single model, and the multiple measures per subject were accounted for by estimating the covariances among measurements within an individual using an unstructured covariance matrix. For all of the immune response measures, global models were first performed to assess the significance of the association between each HLA locus and each of the immune outcomes in the discovery cohort. These global models were followed by additional models, which individually tested the association between the dosage of each HLA four-digit allele and the immune outcomes. Because of the high heterozygosity in the HLA loci, we opted to set our level of significance at p < 0.10. A parallel series of analyses were conducted in the replication cohort to test for associations within HLA loci following global locus-level tests of association.
Results
Characteristics of study cohorts
Table 1 lists demographic characteristics of the discovery (n = 1,071) and replication (n = 1,053) study cohorts. Principal component analysis was utilized to determine racial groupings. The analysis revealed a significant difference (p < 0.0001) between the study cohorts in terms of gender, race, ethnicity, and time since smallpox vaccination. Median ID50 (IQR) vaccinia-specific antibody titers for the two cohorts were 132.6 (78.8, 206.5) and 113.5 (63.0, 190.4) (Table 2). Female subjects had significantly higher neutralizing antibody titers than male subjects [median ID50 discovery cohort 159 (93, 256) vs. 125 (75, 186), p < 0.001; replication cohort 144 (82, 204) vs. 110 (61, 189), p = 0.024]. Total PBMC IFN-γ ELISPOT responses for the two cohorts were 52 (24–88) and 17 (5–37) SFC per 2 × 105 PBMCs. In the discovery cohort, male subjects had higher responses than female subjects [55 (27, 95) vs. 41 (17, 70) SFC per 2 × 105 PBMC, p < 0.001]; however, the observed difference in response [17 (5, 37) vs. 18 (5, 32), SFC per 2 × 105 PBMC, p = 0.29] in the replication cohort did not meet the designated threshold (p < 0.10) for significance. While no significant difference was observed between the two cohorts in IFN-γ secretion levels (p = 0.565), the discovery cohort had significantly higher neutralizing antibody titers, ELISPOT responses, and TNF-α secretion levels (p < 0.0001 for all outcomes) than the replication cohort (Table 2).
Associations of HLA alleles with immune response outcomes
As previously described, we found HLA allele associations with variations in VACV-induced humoral (neutralizing antibody) and cellular (total PBMC IFN-γ ELISPOT, CD8+ IFN-γ ELISPOT, IL-1β, IL-6, IL12p40, IFN-γ, and TNF-α) immune outcomes in 1,071 individuals (discovery cohort) following one dose of smallpox vaccine (Ovsyannikova et al. 2011).
Table 3 shows the overall results for significant associations (p < 0.10) between HLA alleles and humoral immune response outcomes across each separate discovery and replication cohort. The association between the DQB1*03:02 allele (median ID50 discovery cohort 152.0, p = 0.015; replication cohort 134.4, p = 0.010) and higher neutralizing antibody titers was replicated. The B*40:02 allele (median ID50 discovery cohort 108.1, p = 0.119; replication cohort 91.5, p = 0.021) was approaching significance in its association with lower neutralizing antibody titers in both cohorts. Two additional findings of interest were observed: DQB1*06:04 (median ID50 discovery cohort 151.4, p = 0.017; replication cohort 126.4, p = 0.166) and DQB1*06:09 (median ID50 discovery cohort 147.7, p = 0.148; replication cohort 169.7, p = 0.001) alleles may potentially be associated with higher neutralizing antibody titers, although statistical significance thresholds were not met.
Apart from the associations with neutralizing antibody titers, there were three replicated, significant associations between HLA-DRB1 alleles and total PBMC IFN-γ ELISPOT responses (Table 3). Specifically, the DRB1*04:03 allele was associated with lower ELISPOT responses in the discovery and replication cohorts (median SFC discovery cohort 39, p = 0.094; replication cohort 12, p = 0.047). The DRB1*08:01 allele (median SFC discovery cohort 61, p = 0.085; replication cohort 20, p = 0.056) was associated with higher ELISPOT responses in both the discovery and replication cohorts. Notably, the association between the DRB1*15:01 allele with IFN-γ ELISPOT responses (median SFC discovery cohort 50, p = 0.016; replication cohort 18, p = 0.007) and with secreted IFN-γ production was also replicated (median pg/mL discovery cohort 181.7, p = 0.052; replication cohort 203.0, p = 0.014). However, the association observed between the HLA-DRB1*15:01 allele and IFN-γ ELISPOT responses, while found in both discovery and replication cohorts, was in the opposite direction. Likewise, the association found between the HLA-A*34:02 allele and IL-12p40 production was in the opposite direction.
We further examined in an exploratory manner the degree to which individual allelic associations agreed between the discovery and replication cohorts. The results for the individual alleles with potential association (p value < 0.10) were found in either of the two cohorts for neutralizing antibody titers, for ELISPOT (total PBMC IFN-γ ELISPOT and CD8α+ IFN-γ ELISPOT) responses, and for cytokine (IL-6, IFN-γ, IL-12p40, TNF-α, and IL-1β) secretion, including alleles in the following loci: HLA-A, HLA-B, HLA-C, HLA-DQA1, HLA-DRB1, and HLA-DPB1. These alleles are displayed in Supplemental Table 1.
Discussion
It is crucial to understand the genetic basis of smallpox vaccine-induced humoral and cellular immunity i to understand vaccine-induced immunity and to aid in the design of new candidate smallpox vaccines. One important step toward this is the validation of genetic associations through replication studies. The purpose of our study focused on replicating genetic associations previously identified in our discovery population-based smallpox vaccine study. Overall, we successfully replicated, with statistical significance, one allelic association (DQB1*03:02) with VACV-specific neutralizing antibody titers, two allelic associations (DRB1*04:03 and DRB1*08:01) with total PBMC IFN-γ ELISPOT responses, and one allelic association (DRB1*15:01) with IFN-γ secretion. The association of HLA-DRB1*15:01 and HLA-A*34:02 alleles with IFN-γ ELISPOT responses and IL-12p40 secretion, respectively, while found in both cohorts, was in the opposite direction. In addition, four other alleles, with allelic p values between 0.10 and 0.20, were identified as being worthy of additional follow-up because their global locus p values were less than 0.10 when tested for association with neutralizing antibody titers. These alleles included HLA-B*40:02, HLA-DQB1*03:01, *06:04, and *06:09. Further, one allelic association (DQB1*06:02) with IFN-γ secretion was similarly deemed to be worthy of further investigation.
The association between the DQB1*03:02 allele and higher neutralizing antibody titers was successfully replicated in this study, suggesting a role of the DQB1*03:02 molecule in the regulation of antibody response to smallpox vaccine. The influence of the DQB1*03 allele was also observed at the haplotype level, where analysis demonstrated a significant association between the DRB1*04-DQB1*03-DPB1*03 haplotype and rubella vaccine-induced antibody responses in two separate cohorts of healthy children (Ovsyannikova et al. 2009). With regard to the immune response to VACV, strong and robust humoral (antibody) responses are dependent on T cell help. Antigen presenting cells (APC) process and present VACV proteins to CD4+ and CD8+ T helper cells, which undergo activation, differentiation, clonal expansion, and effector functions. Help for B cells is provided by CD4 Th2 cells through co-stimulatory signals with CD40L and production of Th2-type cytokines (IL-4, IL-5). Th1 cells, on the other hand, secret IFN-γ, IL-2, and TNF-α cytokines that are critical for driving cytotoxic T lymphocyte (CTL) activity. The dependence of VACV neutralizing antibody responses on T cell help will be important for future studies of the functional effects of replicated HLA (DQB1*03:02) polymorphisms on hematopoietic cells, including B cells.
Our data show clear evidence of an association between several HLA class II DRB1 alleles with VACV-specific cellular responses. The association of DRB1*04:03 and DRB1*08:01 alleles with lower and higher vaccinia-specific IFN-γ ELISPOT responses, respectively, was observed in both cohorts. This finding suggests a possible effect of the DRB1 alleles in the development of adaptive cellular immune responses to VACV. Likewise, the role of HLA class II (DRB1)-restricted CD4+ T cell long-term memory responses against poxviruses induced by vaccination or infection was recently demonstrated (Calvo-Calle et al. 2007; Kennedy and Poland 2010; Wang et al. 2009). Interestingly, the HLA-DRB1*08 allele has been associated with differential antibody responses to other vaccines, including measles vaccine (Ovsyannikova et al. 2004). Consistent with the above finding, the HLA-DRB1*08 (DRB1*08:04) allele was reported to be associated with hepatitis B vaccine responder phenotype in young Hispanics (Li et al. 2009). The difference in effect of these DRB1*04:03 and DRB1*08:01 alleles on vaccine immune response outcome may be due to differences in vaccine antigens (such as vaccinia, measles, hepatitis B) and, hence, viral-specific antigen processing and presentation. Functional studies that seek to understand the immunologic consequences of antigen presentation by different HLA allelic variants are underway.
Of particular interest is the HLA-DRB1 allele *15:01, which was associated in the discovery cohort with decreased numbers of IFN-γ producing cells assayed by ELISPOT, and significantly decreased production of IFN-γ. Similarly, a study of measles vaccine suggested that the DRB1*15:01 allele was associated with measles vaccine virus-induced IFN-γ secretion (Ovsyannikova et al. 2005). A study of 346 children reported an association of the specific DRB1*15/16-DQB1*06-DPB1*03 haplotype with higher IgG antibody titers to measles vaccine; on the other hand, the same DRB1*15/16-DQB1*06-DPB1*03 haplotype was associated with lower IgG titers to rubella vaccine (Ovsyannikova et al. 2006). The HLA-DRB1*15:01 allele has also been associated with susceptibility to HIV infection (i.e., HLA-B40-DRB1*15:01 haplotype) (Raghavan et al. 2009), survival of Mycobacterium tuberculosis in human macrophages (Singh et al. 2013), and susceptibility to HPV16 infection-related Kazakh esophageal squamous cell carcinoma (Hu et al. 2012). Because each HLA class II molecule presents a slightly different assortment of peptides to CD4+ T cells, it is likely that epitopes within this DRB1*15:01- restricted repertoire contribute to the observed immune profiles. One way to test this hypothesis would be to use VACV to stimulate PBMCs from individuals who carry or do not carry the HLA-DRB1*15:01 allele, and do so in the presence and absence of antibodies that block antigen presentation by the HLA-DRB1*15:01 allele. The cytokine secretion patterns of responding T cells can then be analyzed to examine differences in immune profiles in the presence and absence of HLA-DRB1*15:01-restricted responses. Thus, functional studies are necessary to validate the involvement of specific host genetic polymorphisms in the control of immune responses to VACV and other viruses.
To better understand these replicated HLA associations, it is important to note the differences and similarities between the two cohorts used in this study. Although both cohorts were primarily comprised of male subjects, the discovery cohort contained a larger percentage of females than the replication cohort, causing the two cohorts to differ in terms of gender. Additionally, the discovery cohort contained a higher percentage of African-American and Hispanic subjects than the replication cohort, while less were genetically identified as Caucasian in the discovery cohort than in the replication cohort, causing the two cohorts to be racially distinct. However, the cohorts also differed in their phenotypic responses to smallpox vaccine in all immune measures (ID50, total IFN-γ ELISPOT, CD8+ IFN-γ ELISPOT, IL-6, IL-12p40, TNF-α, IL-1β), except IFN-γ secretion.
Data from this study also show gender differences in humoral immune response to smallpox vaccine. Female subjects, in both the discovery and replication cohorts, had significantly higher VACV-specific neutralizing antibody titers than male subjects. These findings are consistent with data regarding gender and humoral immune response to other vaccines, including influenza vaccine, measles/mumps/rubella vaccine, and hepatitis A and B vaccines (Green et al. 1994; Haralambieva et al. 2013; Klein et al. 2010). Additionally, in the discovery cohort, we observed significantly higher cellular (total PBMC IFN-γ ELISPOT) responses in male subjects, consistent with data regarding RA27/3 rubella vaccine and gender (Mitchell 1999). However, these observed gender differences were not significant in the replication cohort and may be due to the smaller proportion of female subjects included in the replication cohort. Gender differences in response to smallpox vaccine may be explained, in part, by sex steroids. Klein et al. (2010) suggests that by causing the differential production of chemokines and cytokines, sex hormones cause women to have higher Th1, Th2, and Treg responses after vaccination than men. Although data concerning gender and humoral response to vaccines were replicated in this study, further studies need to be conducted to determine whether a gender relationship exists for cellular immune responses to smallpox vaccine or not.
To our knowledge, our study is the first to replicate HLA associations found in our previous population-based smallpox vaccine study in a new cohort of smallpox-immunized subjects. These data suggest that both humoral and cellular (ELISPOT) immune responses to smallpox vaccine are genetically influenced by HLA genes and may have implications for future studies. The large cohort sizes used in this study allowed us to find associations that may have been less apparent if smaller study cohorts were used. However, future replication studies could enroll subjects with similar demographic backgrounds; this would allow us to better analyze associations between demographic data, immune response to smallpox vaccine, and HLA genotype. Despite the differences present between these two cohorts, we were still able to successfully replicate several HLA allelic associations, DQB1*03:02, DRB1*04:03, DRB1*08:01, and DRB1*15:01 (significant in both cohorts), suggesting that these alleles are associated with smallpox vaccine-induced immune responses. Note that one of the alleles, DRB1*15:01, was associated with decreased IFN-γ secretion in both cohorts and was associated with opposite effects on total PBMC IFN-γ ELISPOT results in the two cohorts: a decrease of 2 SFC in the discovery cohort and an increase of 1 SFC in the replication cohort. The differences in total PBMC IFN-γ ELISPOT outcomes are quite small and may or may not be biologically significant.
We acknowledge potential limitations in our study, in particular the different composition of race, gender, and vaccine immune response outcomes between the two study cohorts. All subjects in the discovery cohort were vaccinated with smallpox Dryvax vaccine (prepared from calf lymph), and the study subjects in the replication cohort were vaccinated with smallpox ACAM2000 vaccine (propagated in Vero cells). Although both vaccines are originally from the NYCBH strain and exhibit similar immune responses (Frey et al. 2009), there are differences between the two vaccines that may have impacted our study. Dryvax contains a polyclonal population of viruses that are genetically different from the single clone ACAM2000 virus (Osborne et al. 2007). Dryvax was grown on the skin of calves and may have contained additional adventitious agents that alter immunogenicity. Dryvax is more neurovirulent in animal models (Weltzin et al. 2003). Dilution studies in both vaccinia-naïve and vaccinia-experienced subjects have demonstrated differences in vaccine take-rates, (i.e., induction of a cutaneous reaction (Artenstein et al. 2005; Frey et al. 2002) and, while both vaccines elicit a fourfold rise in neutralizing antibody titer in similar numbers of subjects, the titers in ACAM2000 recipients are ~40 % lower than those in the Dryvax recipients (Frey et al. 2009; Monath et al. 2004; Nalca and Zumbrun 2010). Therefore, the vaccines are comparable and, in some aspects, quite similar, but they are not identical. These differences are likely to have an impact on individual immune responses to the vaccines. Another concern is that HLA typing results used to analyze HLA allelic associations with smallpox vaccine-induced immunity outcomes were obtained for our two cohorts using two different molecular genotyping platforms. Sequence-specific PCR (four-digit level resolution) was used for HLA typing in the discovery cohort, and sequencing that combines the advantage of long-range amplification and a unique genotyping algorithm (six-digit level resolution) (Wang et al. 2012) was utilized for HLA typing in the replication cohort. Another potential limitation is that only individual HLA allelic association analyses were carried out. HLA allele distribution may be influenced by linkage disequilibrium and interactions between diverse HLA genes, other genes, and different SNP-defined alleles that tag HLA alleles; thus, associations between VACV-induced immune outcomes and haplotypes are needed in future studies. Despite these differences and limitations, we found several consistent associations between specific HLA alleles and VACV-induced immune response outcomes.
In our studies of HLA associations with smallpox vaccine-specific immune measures, we enrolled participants from two distinct study cohorts. The discovery of consistent HLA associations between these two cohorts is a major strength of this effort. However, these cohorts differed somewhat on demographic features, and they also differed in their measured immune responses. It is possible that these observed differences might have reduced our ability to detect significant consistent associations between cohorts. It is also possible that the heterozygosity of the HLA loci, with potentially important alleles being observed in relatively few subjects, limited our statistical power to detect associations. Further work in larger cohorts would likely lead to the confirmation of additional alleles that play a role in immune responses induced by vaccination against smallpox.
In conclusion, we were able to successfully replicate several of our strongest HLA allelic associations from our previous study in an independent cohort of smallpox immunized subjects: DQB1*03:02, DRB1*04:03, DRB1*08:01, and DRB1*15:01. These results suggest that HLA class II alleles may contribute substantially to the smallpox vaccine-induced adaptive immunity. Understanding their precise effects on humoral and cellular immune responses to smallpox vaccine can aid in smallpox vaccine development in the future. These replication data provide the basis for functional studies of specific HLA variants found to be associated with inter-individual variability in smallpox vaccine-induced immune responses.
References
Amara RR, Nigam P, Sharma S, Liu J, Bostik V (2004) Long-lived poxvirus immunity, robust CD4 help, and better persistence of CD4 than CD8 T cells. J Virol 78:3811–3816
Artenstein AW, Johnson C, Marbury TC, Morrison D, Blum PS, Kemp T, Nichols R, Balser JP, Currie M, Monath TP (2005) A novel, cell culture-derived smallpox vaccine in vaccinia-naive adults. Vaccine 23:3301–3309
Bhanuprakash V, Hosamani M, Venkatesan G, Balamurugan V, Yogisharadhya R, Singh RK (2012) Animal poxvirus vaccines: a comprehensive review. Expert Rev Vaccines 11:1355–1374. doi:10.1586/erv.12.116
Calvo-Calle JM, Strug I, Nastke MD, Baker SP, Stern LJ (2007) Human CD4+ T cell epitopes from vaccinia virus induced by vaccination or infection. PLoS Pathog 3:1511–1529
de Vries RP, Kreeftenberg HG, Loggen HG, Van Rood JJ (1977) In vitro immune responsiveness to vaccinea virus and HLA. N Engl J Med 297:692–696
Frey SE, Couch RB, Tacket CO, Treanor JJ, Wolff M, Newman FK, Atmar RL, Edelman R, Nolan CM, Belshe RB (2002) Clinical responses to undiluted and diluted smallpox vaccine. N Engl J Med 346:1265–1274
Frey SE, Newman FK, Kennedy JS, Ennis F, Abate G, Hoft DF, Monath TP (2009) Comparison of the safety and immunogenicity of ACAM1000, ACAM2000 and Dryvax in healthy vaccinia-naive adults. Vaccine 27:1637–1644
Green MS, Shohat T, Lerman Y, Cohen D, Slepon R, Duvdevani P, Varsano N, Dagan R, Mendelson E (1994) Sex differences in the humoral antibody response to live measles vaccine in young adults. Int J Epidemiol 23:1078–1081
Haralambieva IH, Ovsyannikova IG, Dhiman N, Kennedy RB, O’Byrne M, Pankrantz VS, Jacobson RM, Poland GA (2011) Common SNPs/haplotypes in IL18R1 and IL18 genes are associated with variations in humoral immunity to smallpox vaccination in caucasians and African-Americans. J Infect Dis 204:433–441
Haralambieva IH, Ovsyannikova IG, Kennedy RB, Larrabee BR, Shane Pankratz V, Poland GA (2013) Race and sex-based differences in cytokine immune responses to smallpox vaccine in healthy individuals. Hum Immunol. doi:10.1016/j.humimm.2013.06.031
Henderson DA (1998) Eradication: lessons from the past. Bull World Health Organ 76(Suppl 2):17–21
Hu J, Li L, Pang L, Chen Y, Yang L, Liu C, Zhao J, Chang B, Qi Y, Liang W, Li F (2012) HLA-DRB1*1501 and HLA-DQB1*0301 alleles are positively associated with HPV16 infection-related Kazakh esophageal squamous cell carcinoma in Xinjiang China. Cancer Immunol Immunother CII 61:2135–2141. doi:10.1007/s00262-012-1281-x
Kennedy RB, Poland GA (2010) The identification of HLA class II-restricted T cell epitopes to vaccinia virus membrane proteins. Virology 408:232–240
Kennedy R, Ovsyannikova IG, Pankratz VS, Vierkant RA, Jacobson RM, Ryan MAK, Poland GA (2008) Gender effects on humoral immune response to smallpox vaccine. Vaccine 27:3319–3323
Kennedy R, Pankratz VS, Swanson E, Watson D, Golding H, Poland GA (2009) Statistical approach to estimate vaccinia-specific neutralizing antibody titers using a high-throughput assay. Clin Vaccine Immunol 16:1105–1112
Kennedy RB, Ovsyannikova IG, Pankratz VS, Haralambieva IH, Vierkant RA, Jacobson RM, Poland GA (2012) Genome-wide genetic associations with IFNgamma response to smallpox vaccine. Hum Genet 131:1433–1451
Klein SL, Jedlicka A, Pekosz A (2010) The Xs and Y of immune responses to viral vaccines. Lancet Infect Dis 10:338–349
Li Y, Ni R, Song W, Shao W, Shrestha S, Ahmad S, Cunningham CK, Flynn PM, Kapogiannis BG, Wilson CM, Tang J (2009) Clear and independent associations of several HLA-DRB1 alleles with differential antibody responses to hepatitis B vaccination in youth. Hum Genet 126:685–696
Manischewitz J, King LR, Bleckwenn NA, Shiloach J, Taffs R, Merchlinsky M, Eller N, Mikolajczyk MG, Clanton DJ, Monath T, Weltzin RA, Scott DE, Golding H (2003) Development of a novel vaccinia-neutralization assay based on reporter-gene expression. J Infect Dis 188:440–448
Mitchell LA (1999) Sex differences in antibody- and cell-mediated immune response to rubella re-immunisation. J Med Microbiol 48:1075–1080
Monath TP, Caldwell JR, Mundt W, Fusco J, Johnson CS, Buller M, Liu J, Gardner B, Downing G, Blum PS, Kemp T, Nichols R, Weltzin R (2004) ACAM2000 clonal Vero cell culture vaccinia virus (New York City Board of Health strain): a second-generation smallpox vaccine for biological defense. Int J Infect Dis 8(Suppl 2):S31–S44
Nalca A, Zumbrun EE (2010) ACAM2000: the new smallpox vaccine for United States Strategic National Stockpile. Drug Des Dev Ther 4:71–79
Narwaney KJ, Glanz JM, Norris JM, Fingerlin TE, Hokanson JE, Rewers M, Hambidge SJ (2013) Association of HLA class II genes with clinical hypo responsiveness to trivalent inactivated influenza vaccine in children. Vaccine 31:1123–1128. doi:10.1016/j.vaccine.2012.12.026
Osborne JD, Da Silva M, Frace AM, Sammons SA, Olsen-Rasmussen M, Upton C, Buller RM, Chen N, Feng Z, Roper RL, Liu J, Pougatcheva S, Chen W, Wohlhueter RM, Esposito JJ (2007) Genomic differences of Vaccinia virus clones from Dryvax smallpox vaccine: the Dryvax-like ACAM2000 and the mouse neurovirulent Clone-3. Vaccine 25:8807–8832
Ovsyannikova IG, Jacobson RM, Vierkant RA, Pankratz SV, Jacobsen SJ, Poland GA (2004) Associations between human leukocyte antigen (HLA) alleles and very high levels of measles antibody following vaccination. Vaccine 22:1914–1920
Ovsyannikova IG, Jacobson RM, Ryan JE, Vierkant RA, Pankratz VS, Jacobsen SJ, Poland GA (2005) HLA class II alleles and measles virus-specific cytokine immune response following two doses of measles vaccine. Immunogenetics 56:798–807
Ovsyannikova IG, Pankratz VS, Vierkant RA, Jacobson RM, Poland GA (2006) Human leukocyte antigen haplotypes in the genetic control of immune response to measles-mumps-rubella vaccine. J Infect Dis 193:655–663
Ovsyannikova IG, Jacobson RM, Vierkant RA, O’Byrne MM, Poland GA (2009) Replication of rubella vaccine population genetic studies: validation of HLA genotype and humoral response associations. Vaccine 27:6926–6931
Ovsyannikova IG, Vierkant RA, Pankratz VS, Jacobson RM, Poland GA (2011) Human leukocyte antigen genotypes in the genetic control of adaptive immune responses to smallpox vaccine. J Infect Dis 203:1546–1555
Ovsyannikova IG, Haralambieva IH, Kennedy RB, Pankratz VS, Vierkant RA, Jacobson RM, Poland GA (2012a) Impact of cytokine and cytokine receptor gene polymorphisms on cellular immunity after smallpox vaccination. Gene 510:59–65
Ovsyannikova IG, Kennedy RB, O’Byrne M, Jacobson RM, Pankratz VS, Poland GA (2012b) Genome-wide association study of antibody response to smallpox vaccine. Vaccine 30:4182–4189
Ovsyannikova IG, Haralambieva IH, Kennedy RB, O’Byrne MM, Pankratz VS, Poland GA (2013a) Genetic variation in IL18R1 and IL18 genes and interferon gamma ELISPOT response to smallpox vaccination: an unexpected relationship. J Infect Dis 208:1422–1430. doi:10.1093/infdis/jit341
Ovsyannikova IG, Pankratz VS, Vierkant RA, Pajewski NM, Quinn CP, Kaslow RA, Jacobson RM, Poland GA (2013b) Human leukocyte antigens and cellular immune responses to anthrax vaccine adsorbed. Infect Immun 81:2584–2591. doi:10.1128/IAI.00269-13
Pajewski NM, Parker SD, Poland GA, Ovsyannikova IG, Song W, Zhang K, McKinney BA, Pankratz VS, Edberg J, Kimberly RP, Jacobson RM, Tang J, Kaslow RA (2011) The role of HLA DR-DQ haplotypes in variable antibody responses to anthrax vaccine adsorbed. Genes Immun 12:457–465
Poland GA, Ovsyannikova IG, Jacobson RM, Smith DI (2007) Heterogeneity in vaccine immune response: the role of immunogenetics and the emerging field of vaccinomics. Clin Pharmacol Ther 82:653–664
Raghavan S, Selvaraj P, Swaminathan S, Alagarasu K, Narendran G, Narayanan PR (2009) Haplotype analysis of HLA-A, -B antigens and -DRB1 alleles in south Indian HIV-1-infected patients with and without pulmonary tuberculosis. Int J Immunogenet 36:129–133. doi:10.1111/j.1744-313X.2009.00835.x
Singh AK, Abhimanyu, Yadav AB, Sharma S, Garg R, Bose M, Misra A (2013) HLA-DRB1*1501 and VDR polymorphisms and survival of Mycobacterium tuberculosis in human macrophages exposed to inhalable microparticles. Pharmacogenomics 14:531–540. doi:10.2217/pgs.13.12
Verardi PH, Titong A, Hagen CJ (2012) A vaccinia virus renaissance: new vaccine and immunotherapeutic uses after smallpox eradication. Hum Vaccines Immunother 8:961–970. doi:10.4161/hv.21080
Walsh SR, Dolin R (2011) Vaccinia viruses: vaccines against smallpox and vectors against infectious diseases and tumors. Expert Rev Vaccines 10:1221–1240. doi:10.1586/erv.11.79
Wang M, Tang ST, Lund O, Dziegiel MH, Buus S, Claesson MH (2009) High-affinity human leucocyte antigen class I binding variola-derived peptides induce CD4+ T cell responses more than 30 years post-vaccinia virus vaccination. Clin Exp Immunol 155:441–446. doi:10.1111/j.1365-2249.2008.03856.x
Wang C, Krishnakumar S, Wilhelmy J, Babrzadeh F, Stepanyan L, Su LF, Levinson D, Fernandez-Vina MA, Davis RW, Davis MM, Mindrinos M (2012) High-throughput, high-fidelity HLA genotyping with deep sequencing. Proc Natl Acad Sci USA 109:8676–8681
Weltzin R, Liu J, Pugachev KV, Myers GA, Coughlin B, Blum PS, Nichols R, Johnson C, Cruz J, Kennedy JS, Ennis FA, Monath TP (2003) Clonal vaccinia virus grown in cell culture as a new smallpox vaccine. Nat Med 9:1125–1130
Acknowledgments
We thank the Mayo Clinic Vaccine Research Group in Rochester, Minnesota, the Naval Health Research Center in San Diego, California, and the subjects who participated in our studies. We thank Beth R. Larrabee for her assistance in statistical analysis. We thank Caroline L. Vitse for her editorial assistance. This project was funded by federal funds from the National Institute of Allergies and Infectious Diseases, National Institutes of Health, Department of Health and Human Services, under Contract No. HHSN272201000025C (N01AI40065). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest
Dr. Poland is the chair of a Safety Evaluation Committee for novel non-vaccinia investigational vaccine trials being conducted by Merck Research Laboratories. Dr. Poland offers consultative advice on vaccine development to Merck & Co. Inc., CSL Biotherapies, Avianax, Sanofi Pasteur, Dynavax, Novartis Vaccines and Therapeutics, PAXVAX Inc, and Emergent Biosolutions. Drs. Poland and Ovsyannikova hold two patents related to vaccinia and measles peptide research. These activities have been reviewed by the Mayo Clinic Conflict of Interest Review Board and are conducted in compliance with Mayo Clinic Conflict of Interest policies. This research has been reviewed by the Mayo Clinic Conflict of Interest Review Board and was conducted in compliance with Mayo Clinic Conflict of Interest policies.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ovsyannikova, I.G., Pankratz, V.S., Salk, H.M. et al. HLA alleles associated with the adaptive immune response to smallpox vaccine: a replication study. Hum Genet 133, 1083–1092 (2014). https://doi.org/10.1007/s00439-014-1449-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00439-014-1449-x