Abstract
A disadvantage in Q fever diagnostics and research is the insensitive and difficult culture of Coxiella burnetii. This intracellular organism can only be isolated using embryonated eggs, animal hosts, or mammalian cell culture. In consequence, it has only been possible to isolate a few strains from human patients. Here, we describe the first isolation of C. burnetii from a clinical specimen using the recently developed cell-free medium acidified citrate cysteine medium 2 (ACCM2). We screened the sera of 217 patients who had undergone valvular transplantation but detected one serum with an antibody constellation indicating chronic Q fever. Polymerase chain reaction (PCR) of the corresponding heart valve revealed 3.1 × 105 copies/rxn. The strain was successfully isolated using ACCM2. Genomic investigation by multilocus variable-number of tandem repeat (VNTR) analysis (MLVA) revealed the strain to be a new genotype, A10, closely related to one from sheep. As the sensitivity of ACCM2 for different human strains is unknown, we also investigated combining a robust test, egg propagation, with ACCM2. This combination produced four to six logs of growth of the bacteria. The use of ACCM2 in this combination simplified the otherwise elaborate purification steps. Cultivation in ACCM2 has the potential to simplify the isolation of C. burnetii in a clinical setting. As the success rates of cell culture for virulent C. burnetii strains are variable, the sensitivity of ACCM2 for different strains is unknown, and many specimens may contain much fewer bacteria than in our case, the combination of the robust method of egg propagation with ACCM2 is a good alternative to existing single methods for investigating critical specimens.
Similar content being viewed by others
Introduction
Coxiella burnetii is the pathogen causing Q fever and is an obligate intracellular bacterium in nature. Q fever occurs in outbreaks of flu-like illnesses, with potential complications such as pneumonia. The source of human infection is most commonly identified as birth matter from ruminants, whether abortions or natural births. Inhaling small-particle aerosols of such material containing C. burnetii is the typical method by which humans become infected.
Of people with acute Q fever, 1–5 % develop a chronic infection, the most usual such infection being a culture-negative endocarditis [1–3]. The chronic disease can be fatal if it is not treated appropriately. Chronic Q fever should be suspected where prolonged elevated IgG phase I (Ph1-IgG) antibodies (≥1:1,024) are recorded [4, 5].
An existing difficulty in the diagnosis of Q fever, and in research and risk assessment, is the insensitive, lengthy, and difficult culture of C. burnetii. Only a few strains have been isolated from human samples so far. However, because C. burnetii is an intracellular organism, it is generally only possible to identify it from clinical specimens by culturing it in embryonated eggs, animal hosts, or cultures of mammalian cells. Hen egg propagation is a particularly effective method for producing large amounts of Coxiella [6] and, thus, overcoming the problem of small pathogen numbers in specimens. But these methods have disadvantages, e.g., several purification steps are necessary to achieve material applicable for further investigations [7]. In addition, all work must be performed under biosafety level 3 laboratory conditions.
A milestone in C. burnetii research was reached in 2009 by the development of an axenic culture system for this formerly obligate intracellular bacterium [8]. This system, acidified citrate cysteine medium (ACCM) was created based on information from acid activation studies, together with analyses using transcription microarray techniques, metabolic pathway reconstruction, and metabolite typing. Two years later, it was optimized to ACCM2 [9].
We tested this new axenic culture medium alone and in combination with the robust hen egg propagation method for isolating C. burnetii from clinical specimens.
Materials and methods
Heart valves and sera from patients who had undergone heart valve transplantation at our hospital are subjected to routine microbiological diagnostics in our department. They are then stored at −25 °C in case further investigation is required. We screened for chronic Q fever all available sera corresponding to heart valves collected between October 2007 and December 2012. We screened by performing an indirect fluorescent antibody test (Focus/Genzyme-Virotech, Rüsselsheim, Germany). We took Ph1-IgG titer ≥1:1,024 as indicating chronic C. burnetii infection.
Only one heart valve out of 217 corresponded to serum with antibody titer indicating chronic infection. We ground this valve with 3 ml of phosphate-buffered saline (PBS). This yielded a suspension of tissue in PBS, “suspension”, and also the remnant heart valve “valve”. It was not necessary for us to filter the suspension because the routine microbiological investigation had not revealed any other pathogen. Then, we performed direct incubation of the valve in ACCM2. The suspension was further investigated by polymerase chain reaction (PCR), hen egg propagation with subsequent ACCM2 incubation, and Buffalo green monkey cell culture (BGM cells), as described below.
Polymerase chain reaction for Coxiella burnetii
In general, the DNA was extracted from 200 μl of specimen using the QIAamp Blood Kit (Qiagen, Hilden, Germany), as described by the manufacturer. For the DNA extraction from the original suspension, the protocol was modified to 500 μl of suspension and 50 μl of AE buffer to elute the DNA to increase the sensitivity. This modification was taken into account when we calculated the C. burnetii concentrations. The following real-time PCR (LightMix® for the detection of Coxiella burnetii, TIB Molbiol, Berlin, Germany) targets the IS1111 and com1 gene and was performed using LightCycler® FastStart DNA Master HybProbe (Roche Diagnostics, Mannheim, Germany) and LightCycler 2.0 (Roche Diagnostics, Mannheim, Germany), according to the instructions of the manufacturer (template of 5 μl). The standard row, supplied with the kit, of cloned DNA with concentrations in the range from 106 copies/rxn to 101 copies/rxn of C. burnetii was used for quantification.
16S rDNA PCR
DNA was extracted from ACCM2-Agarose using the QIAamp Blood Kit (Qiagen, Hilden, Germany), as described by the manufacturer. To confirm the basic PCR conditions, negative, positive, and inhibition controls were done for each sample. Different primer pairs were used for Gram-negative and Gram-positive bacteria. The pair used for Gram-negatives was F 5′TggTAgTCCACgCCgTAAACg3′, R CgTAAgggCCATgATgACT3′ and that for Gram-positives was F 5′TggTAgTCCACgCCgTAAACg3′, R 5′TCATAAggggCATgATgAT3′. The amplification conditions were as follows: an initial denaturation step at 95 °C for 900 s, followed by 35 cycles of denaturation at 94 °C for 15 s, annealing at 53 °C for 15 s, extension at 72 °C for 60 s, and terminal elongation at 72 °C for 300 s. The product was sequenced with an ABI PRISM 310 DNA sequencer (Applied Biosystems). Sequence associations were determined by using the BLAST search algorithm of the GenBank database (National Center for Biotechnology Information).
Hen egg propagation
We used ten specific pathogen-free hen eggs (SPF eggs from Charles River Laboratories, Sulzfeld, Germany) and injected 200 μl of the suspension into each egg. The eggs were maintained in an egg incubator at 39 °C with 58–60 % relative humidity [7]. After 7 days, or earlier if the hen embryo died, 1 ml of each yolk was transferred to 29 ml of ACCM2 medium.
Acidified citrate cysteine medium 2 (ACCM2)
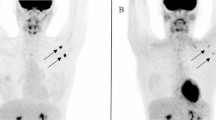
ACCM2 was prepared as described by Omsland et al. and transferred to T25 cell culture flasks (Greiner Bio-One GmbH, Frickenhausen, Germany) [10]. The remaining 600 μl lump of valve tissue was incubated in ACCM2 with an end volume of 20 ml and approximately 1 ml of the harvested yolks was incubated with 29 ml of ACCM2 (Fig. 1), all of them at 37 °C in a 2.5 % O2 and 5 % CO2 environment using a CO-170 incubator (New Brunswick Scientific, New Brunswick, NJ, USA). Unfortunately, agitation at 75 rpm as recommended could not be achieved [10]. A large plastic photo tray filled with distilled water was put into the incubator to prevent the medium evaporating.
Acidified citrate cysteine medium 2-agarose (ACCM2-Agarose)
ACCM2-Agarose was prepared as described but without the thin overlay of medium recommended [11].
For PCR, we harvested ~200 μl of the yolks, 200 μl of ACCM2 containing the valve on days 6, 7, 8, and 15, and 200 μl of the ACCM2 containing the infected yolks on day 15 of the whole cultivation time (including the time of egg propagation). Of the ACCM2 incubating the valve, 100 μl were transferred to an ACCM2-Agarose plate and incubated for 7 days in a 2.5 % oxygen environment. The plate was inspected macroscopically and by phase contrast microscopy every day after the first 5 days of incubation.
For better comparison, we adjusted the PCR results to the original concentration in the suspension. To do this, we multiplied the results of the yolk PCR for days 1–5 by 20 (200 μl of the suspension were injected and the yolks had a final volume of 4 ml) and for days 7–10 (when the consumption of yolk by the embryo had reduced the yolks to ~2 ml). The results from day 14 of ACCM2 incubation together with egg propagation were adjusted to the original concentration in suspension by multiplication by 600 for days 1–5 (1 ml out of a 4-ml yolk, infected with 200 μl of suspension, were made up to 30 ml with ACCM2) and by multiplication by 300 for day 7 (yolks reduced to 2 ml). We were unable to extract DNA from a homogenized heart tissue because suitable tools for work under biosafety level 3 were lacking. Therefore, we did not adjust the results of the direct incubation of the valve tissue in ACCM2 to the value in the original heart valve.
Buffalo green monkey cell culture (BGM cells)
For intracellular growth, BGM cells in UltraCulture, 1 % NEAA, 1 % Modified Eagle’s Medium Essential Vitamin Mixture, and 2 mmol L-glutamine (Lonza BioWhittaker®, Verviers, Belgium) were plated in two T25 flasks and 500 μl of the suspension was added. These flasks were then incubated at 37 °C in 5 % CO2 environment.
In order to detect vacuoles, the flasks were examined daily by phase contrast microscopy after the first 5 days.
Genomic characterization
The identification of plasmid type, adaA variant and multilocus variable-number of tandem repeat (VNTR) analysis (MLVA) genotype was performed according to published methods [12, 13].
Results
We detected only one patient of 217 with a serum Ph1-IgG titer of more than 1:1,024. Dilution of the serum revealed a Ph1-IgG titer of more than 1:65,536. The patient had suffered from severe mitral valve insufficiency and received a bioprosthetic valve in 2005. The original valve had been investigated by routine microbiological methods, but they had not detected any culturable pathogen.
PCR of the suspension indicated 3.1 × 105 genome copies/rxn of C. burnetii. The analyses of ACCM2 cultures (20 ml) containing the valve showed an increasing amount of C. burnetii from 8.1 × 103 to 1.4 × 105 genome copies/rxn (equivalent to 5 μl) between day 6 and day 8 of incubation (Fig. 1). There was no significant reduction of ACCM2 volume through evaporation. The ACCM2-Agarose plate inoculated with 100 μl of the positive ACCM2 after incubation of the valve showed several small colonies on day 5. These colonies grew inside the agarose gel and could be seen by phase contrast microscopy. These colonies were confirmed as being C. burnetii by 16S rDNA PCR.
Of the infected eggs, four died on day 1, one on day 2, and two on day 5. Three eggs survived until day 7. PCR of the yolks indicated 1.67 × 104–6.28 × 105 genome copies/rxn for day 1, 2.64 × 105 genome copies/rxn for day 2, 3.2 × 108–5.04 × 108 genome copies/rxn for day 5, and 1.57 × 109–5.5 × 109 genome copies/rxn for day 7, when adjusted to the original PBS suspension of the heart valve (Fig. 1).
On day 14 of ACCM2 incubation combined with egg propagation, 4.3 × 109–1.7 × 1011 genome copies/rxn were found by PCR adjusted to the original concentration in heart valve PBS (Fig. 1). In combination, these data show four to six logs growth over 14 days.
Few vacuoles characteristic of C. burnetii in cell culture were detectable by phase contrast microscopy on day 6.
Further genomic characterization by MLVA revealed a new genotype, A10. This genotype is closely related to the A3 type found in one isolate from a sheep in 1998 and from another sheep in 2010 in south-west Germany. The new allele pattern in the 14 markers is as follows (repeat number given in brackets): ms01 (4), ms03 (7), ms20 (18), ms21 (6), ms22 (6), ms23 (3), ms24 (9), ms26 (9), ms27 (3), ms28 (3), ms30 (5), ms31 (2), ms33 (5), and ms34 (5).
In addition, the isolate contained the very common QpH1 plasmid and was of the adaA wild type.
Discussion
A major problem in Q fever research is the limited number of C. burnetii strains isolated from patients. Suitable specimens of infected tissue from human patients are rare and usually only available as a result of invasive procedures such as heart valve replacement or bronchoalveolar lavage. A further problem is that there is no routine method for propagating C. burnetii. Only specialized laboratories perform cell culture or animal/hen egg propagation under biosafety level 3 conditions. These problems are reflected in the fact that, as yet, only one strain has been isolated from human samples in Germany.
Our data show, for the first time, success in a clinical setting of the recently developed cell-free medium ACCM2, a potential alternative to the laborious methods currently used.
We identified only one person (among 217 patients) with an antibody titer suggesting chronic Q fever. Examination of the heart valve of this patient revealed high numbers of bacteria.
An increase in the numbers of bacteria ranging from 8.1 × 103 on day 6 to 1.4 × 105 per rxn (5 μl) on day 8 of incubation, corresponding to only four cell divisions in 2 days, was found in ACCM2 containing the valve. Unfortunately, we only started to sample on day 6, which may be after the proliferation stage of the bacteria. An inoculum of 1.0 × 106 bacteria/ml entered the stationary phase in approximately 6 days [9]. However, we were able to exclude evaporation effects because the volume remained stable and the culture was suitable for genomic characterization. Furthermore, the bacteria were even able to grow subsequently on ACCM2-Agarose plates. Even in earlier experiments, we had been able to grow C. burnetii on ACCM2-Agarose without the thin overlayer recommended. After inoculation with 100 μl of ACCM2 containing the bacteria, the surface is completely covered with fluid. Because we immediately transferred the plates to the incubator and ensured high humidity in the incubator, it is likely that C. burnetii has sufficient moisture and ACCM2 provides the right pH for proper membrane function and stability to grow into the 0.25 % ACCM2-Agarose. We found that C. burnetii colonies do not grow directly on the surface of solid ACCM2 but, indeed, as has been reported previously [9], grow within it.
The new genotype, A10, is closely related to the A3 type associated with sheep. However, the patient from whom the C. burnetii were isolated did not report frequent contact with animals. Nevertheless, the genomic similarity is in line with the fact that the majority of Q fever cases in Germany are sheep associated [14–16].
A high bacterial concentration of up to 108 bacteria/rxn was found in ACCM2 after hen egg propagation. These concentrations were unrelated to the duration of egg propagation. However, it is difficult to separate the yolks from other tissues in the egg. Several of the yolks harvested were consequently incomplete and their volume had to be estimated. Keeping this in mind, the four to six logs growth found in our study correspond well with the four to five logs growth of virulent C. burnetii strains found by Omsland et al., even though we were unable to agitate the culture [10].
Egg propagation of C. burnetii is known to be a robust and reliable method. It is burdened, however, with its requirement for hazardous laboratory handling. We have shown, however, that combining egg propagation with ACCM2 culture is successful, and that it avoids the time-consuming and laborious purification otherwise required for additional molecular biological tests.
We also found growth in cell culture, which is a well-established enrichment method for C. burnetii. Cell culture has fewer biosafety problems than egg propagation, but has a very variable success rate for the isolation of strains of different virulence [17, 18]. The low infectivity of virulent phase I C. burnetii for cells in culture seems to be attributable to the hydrophilic nature of phase I C. burnetii. They are hydrophilic because of their coating of O-antigen sugars. These unspecifically inhibit interactions with the host cell plasma membrane. There is no such inhibition with the phase II organisms because their truncated lipopolysaccharides make them hydrophobic [19]. The hydrophilicity of phase I C. burnetii has, of course, no relevance in ACCM2 because it is a cell-free medium. The absence of inhibition is, thus, a particular advantage for this medium [9].
ACCM2 is highly sensitive for isolating the avirulent C. burnetii strain NMII from animal tissue at an initial genome equivalent of 10, but NMII was the reference strain during the development of ACCM2 [10]. However, sensitivity may differ between strains. For example, of six different C. burnetii strains, four increased 1,000-fold, one only 100-fold, and one grew poorly in ACCM, the forerunner of ACCM2 [20]. As yet, there is no information on the sensitivity to ACCM2 of different human strains.
In conclusion, we were able, for the first time, to isolate C. burnetii from clinical specimens by using ACCM2. We, therefore, believe that ACCM2 has the potential to simplify and increase the rate of isolation of pathogenic C. burnetii strains. However, the sensitivity of ACCM2 for different human strains is unknown and specimens may well contain many fewer bacteria than the heart valve we investigated. Therefore, egg propagation is still an appropriate choice for the robust investigation of limited and, therefore, valuable samples of human tissue. We were also able to determine that egg propagation can be combined with ACCM2, and this obviously simplifies purification of the bacteria. The strain we isolated was of a new genotype, A10, which is closely related to sheep-derived isolates, reflecting the fact that the majority of Q fever cases in Germany are sheep related. We found that ACCM2-Agarose plates worked well without the recommended overlayer. It must be noted that ACCM2 must be cultured in a reduced oxygen environment and, therefore, a special incubator is needed. This limits the broader application of this method as, indeed, does the requirement of this work for a biosafety 3 laboratory. An axenic medium has been developed recently for growing Chlamydia trachomatis in a reduced oxygen environment [21]. The development of axenic media for other intracellular bacteria would be very welcome because it would increase the efficiency of detecting such bacteria in diagnostic laboratories.
References
Fenollar F, Fournier PE, Carrieri MP, Habib G, Messana T, Raoult D (2001) Risks factors and prevention of Q fever endocarditis. Clin Infect Dis 33(3):312–316
Maurin M, Raoult D (1999) Q fever. Clin Microbiol Rev 12(4):518–553
Landais C, Fenollar F, Thuny F, Raoult D (2007) From acute Q fever to endocarditis: serological follow-up strategy. Clin Infect Dis 44(10):1337–1340
Dupont HT, Thirion X, Raoult D (1994) Q fever serology: cutoff determination for microimmunofluorescence. Clin Diagn Lab Immunol 1(2):189–196
Kampschreur LM, Oosterheert JJ, Koop AM, Wegdam-Blans MC, Delsing CE, Bleeker-Rovers CP, De Jager-Leclercq MG, Groot CA, Sprong T, Nabuurs-Franssen MH, Renders NH, van Kasteren ME, Soethoudt Y, Blank SN, Pronk MJ, Groenwold RH, Hoepelman AI, Wever PC (2012) Microbiological challenges in the diagnosis of chronic Q fever. Clin Vaccine Immunol 19(5):787–790
Williams JC, Peacock MG, McCaul TF (1981) Immunological and biological characterization of Coxiella burnetii, phases I and II, separated from host components. Infect Immun 32(2):840–851
Samuel JE, Hendrix LR (2009) Laboratory maintenance of Coxiella burnetii. Curr Protoc Microbiol Chapter 6:Unit 6C.1
Omsland A, Cockrell DC, Howe D, Fischer ER, Virtaneva K, Sturdevant DE, Porcella SF, Heinzen RA (2009) Host cell-free growth of the Q fever bacterium Coxiella burnetii. Proc Natl Acad Sci U S A 106(11):4430–4434
Omsland A (2012) Axenic growth of Coxiella burnetii. Adv Exp Med Biol 984:215–229
Omsland A, Beare PA, Hill J, Cockrell DC, Howe D, Hansen B, Samuel JE, Heinzen RA (2011) Isolation from animal tissue and genetic transformation of Coxiella burnetii are facilitated by an improved axenic growth medium. Appl Environ Microbiol 77(11):3720–3725
Cursons RT, Jeyerajah E, Sleigh JW (1999) The use of polymerase chain reaction to detect septicemia in critically ill patients. Crit Care Med 27(5):937–940
Frangoulidis D, Walter MC, Antwerpen M, Zimmermann P, Janowetz B, Alex M, Böttcher J, Henning K, Hilbert A, Ganter M, Runge M, Münsterkötter M, Splettstoesser WD, Hanczaruk M (2014) Molecular analysis of Coxiella burnetii in Germany reveals evolution of unique clonal clusters. Int J Med Microbiol 304(7):868–876
Frangoulidis D, Splettstoesser WD, Landt O, Dehnhardt J, Henning K, Hilbert A, Bauer T, Antwerpen M, Meyer H, Walter MC, Knobloch JK (2013) Microevolution of the chromosomal region of acute disease antigen A (adaA) in the query (Q) fever agent Coxiella burnetii. PLoS One 8(1):e53440
Gilsdorf A, Kroh C, Grimm S, Jensen E, Wagner-Wiening C, Alpers K (2008) Large Q fever outbreak due to sheep farming near residential areas, Germany, 2005. Epidemiol Infect 136(8):1084–1087
Hellenbrand W, Breuer T, Petersen L (2001) Changing epidemiology of Q fever in Germany, 1947–1999. Emerg Infect Dis 7(5):789–796
Porten K, Rissland J, Tigges A, Broll S, Hopp W, Lunemann M, van Treeck U, Kimmig P, Brockmann SO, Wagner-Wiening C, Hellenbrand W, Buchholz U (2006) A super-spreading ewe infects hundreds with Q fever at a farmers’ market in Germany. BMC Infect Dis 6:147
Gouriet F, Fenollar F, Patrice JY, Drancourt M, Raoult D (2005) Use of shell-vial cell culture assay for isolation of bacteria from clinical specimens: 13 years of experience. J Clin Microbiol 43(10):4993–5002
Spyridaki I, Gikas A, Kofteridis D, Psaroulaki A, Tselentis Y (1998) Q fever in the Greek island of Crete: detection, isolation, and molecular identification of eight strains of Coxiella burnetii from clinical samples. J Clin Microbiol 36(7):2063–2067
Voth DE, Heinzen RA (2007) Lounging in a lysosome: the intracellular lifestyle of Coxiella burnetii. Cell Microbiol 9(4):829–840
Kersh GJ, Oliver LD, Self JS, Fitzpatrick KA, Massung RF (2011) Virulence of pathogenic Coxiella burnetii strains after growth in the absence of host cells. Vector Borne Zoonotic Dis 11(11):1433–1438
Omsland A, Sager J, Nair V, Sturdevant DE, Hackstadt T (2012) Developmental stage-specific metabolic and transcriptional activity of Chlamydia trachomatis in an axenic medium. Proc Natl Acad Sci U S A 109(48):19781–19785
Acknowledgments
This work was supported by the Federal Ministry of Education and Research (BMBF), Germany (Katharina Boden, Dimitrios Frangoulidis, grant KI 1001C). We thank Juliana Schrimpf and Beate Haschke for her technical support in the laboratory.
Conflict of interest
The authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boden, K., Wolf, K., Hermann, B. et al. First isolation of Coxiella burnetii from clinical material by cell-free medium (ACCM2). Eur J Clin Microbiol Infect Dis 34, 1017–1022 (2015). https://doi.org/10.1007/s10096-015-2321-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-015-2321-1