ABSTRACT
Purpose
To clarify relationships among various types of target-mediated disposition (TMD) models including the Michaelis-Menten, quasi-steady-state (Qss), and rapid binding models and propose measures for the closeness of some models as approximations to the general TMD model (Mager and Jusko, J Pharmacokinet Pharmacodyn 28(6):507–532, 2001).
Methods
Based on the classic singular perturbation theory by selecting appropriate scales of time, we derive requirements with which the Michaelis-Menten and Qss models are suitable approximations. Under the Qss assumption we show that other simplifications of the general TMD model can be similarly obtained as the Michaelis-Menten and Qss models. We compare these models by simulations using known application examples.
Results
The Michaelis-Menten and Qss models are direct simplifications of the general TMD model and, moreover, suitable approximations if certain specific requirements on the parameters are met.
Conclusions
As a first attempt to quantify the closeness of some simplifications to the general TMD model, our work should provide a more rigorous basis for the theoretical and practical research of TMD models, which are important for investigating the pharmacokinetic-pharmacodynamic relationships of many biological compounds.







Similar content being viewed by others
REFERENCES
Mager D, Jusko W. General pharmacokinetic model for drugs exhibiting target-mediated drug disposition. J Pharmacokinet Pharmacodyn. 2001;28(6):507–32.
Woo S, Krzyzanski W, Jusko W. Target-mediated pharmacokinetic and pharmacodynamic model of recombinant human erythropoietin (rHuEPO). J Pharmacokinet Pharmacodyn. 2007;34:849–68.
Krzyzanski W, Wiczling P, Lowe P, Pigeolet E, Fink M, Berghout A, et al. Population modeling of filgrastim PK-PD in healthy adults following intravenous and subcutaneous administrations. J Clin Pharmacol. 2010;50(9 suppl):101S–12S.
Jin F, Krzyzanski W. Pharmacokinetic model of target-mediated disposition of thrombopoietin. AAPS PharmSci. 2004;6(1) Article 9.
Mager D, Jusko W. Receptor-mediated pharmacokinetic pharmacodynamic model of interferon-β 1a in humans. Pharm Res. 2002;19(10):1537–43.
Eppler S, Combs D, Henry T, Lopez J, Ellis S, Yi JH, et al. A target-mediated model to describe the pharmacokinetics and hemodynamic effects of recombinant human vascular endothelial growth factor in humans. Clin Pharmacol Ther. 2002;72(1):20–32.
Dirks N, Meibohm B. Population pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49:633–59.
Levy G. Pharmacologic target-mediated drug disposition. Clin Pharmacol Ther. 1994;56:248–52.
Hayashi N, Tsukamoto Y, Sallas W, Lowe P. A mechanism-based binding model for the population pharmacokinetics and pharmacodynamics of omalizumab. Br J Clin Pharmacol. 2007;63(5):548–61.
Bauer R, Dedrick R, White M, Murray M, Garovoy M. Population pharmacokinetics and pharmacodynamics of the anti-CD11a antibody hu1124 in human subjects with psoriasis. J Pharmacokinet Pharmacodyn. 1999;27(4):397–420.
Gibiansky L, Gibiansky E. Target-mediated drug disposition model: approximations, identifiability of model parameters and applications to the population pharmacokinetic and pharmacodynamic modeling of biologics. Expert Opin Drug Metab Toxicol. 2009;5(7):803–12.
Mager D, Krzyzanski W. Quasi-equilibrium pharmacokinetic model for drugs exhibiting target-mediated drug disposition. Pharm Res. 2005;22(10):1589–96.
Gibiansky L, Gibiansky E, Kakkar T, Ma P. Approximations of the target-mediated drug disposition model and identifiability of model parameters. J Pharmacokinet Pharmacodyn. 2009;35:573–91.
Peletier L, Gabrielsson J. Dynamics of target-mediated drug disposition. European J Pharm Sci. 2009;38:445–64.
Jonsson E, Macintyre F, James I, Krams M, Marshall S. Bridging the pharmacokinetics and pharmacodynamics of UK-279,276 across healthy volunteers and stroke patients using a mechanistically based model for target-mediated disposition. Pharm Res. 2005;22:1236–46.
Klonowski W. Simplifying principles for chemical and enzyme reaction kinetics. Biophy Chem. 1983;18:73–83.
Segel L, Slemrods M. The quasi-steady-state assumption: a case study in perturbation. SIAM Rev. 1989;31(3):446–77.
Segel I. Enzyme kinetics: behavior and analysis of rapid equilibrium and steady-state enzyme systems. New York: Wiley; 1975.
Yan X, Mager D, Krzyzanski W. Selection between Michaelis-Menten and target-mediated drug disposition pharmacokinetic models. J Pharmacokinet Pharmacodyn. 2010;37:25–47.
Wang W, Wang E, Balthasar J. Monoclonal antibody pharmacokinetics and pharmacodynamics. Clin Pharmacol Ther. 2008;84(5):548–58.
van Bueren JJ Lammerts, Bleeker WK, Bøgh HO, Houtkamp M, Schuurman J, van de Winkel JGJ, et al. Effect of target dynamics on pharmacokinetics of a novel therapeutic antibody against the epidermal growth factor receptor: implications for the mechanisms of action. Cancer Res. 2006;66(15):7630–8.
R Development Core Team. R: a language and environment for statistical computing. Vienna, Austria; 2010. ISBN 3-900051-07-0. Available from: http://www.R-project.org.
Setzer RW. odesolve: Solvers for ordinary differential equations; 2008. R package version 0.5-20.
Ng C, Stefanich E, Anand B, Fielder P, Vaickus L. Pharmacokinetics/pharmacodynamics of nondepleting anti-CD4 monoclonal antibody (TRX1) in healthy human volunteers. Pharm Res. 2006;23(1):95–103.
Marathe A, Peterson M, Mager D. Integrated cellular bone homeostasis model for denosumab pharmacodynamics in multiple myeloma patients. J Pharmacol Exp Ther. 2008;326:555–62.
Kakkar T, Sung C, Gibiansky L, Vu T, Narayanan A, Lin SL, et al. Population PK and IgE pharmacodynamic analysis of a fully human monoclonal antibody against IL4 receptor. Pharm Res. 2011;19(10):1537–43.
Gibiansky L, Sutjandra L, Doshi S, Zheng J, Sohn W, Peterson M, et al. Population pharmacokinetic analysis of denosumab in advanced cancer patients with solid tumors. In: American Conference of Pharmacometrics. San Diego, CA; 2011.
Gibiansky L, Gibiansky E. Irreversible binding (IB) and Michaelis-Menten (MM) approximations of the target-mediated drug disposition (TMDD) model. In: AAPS National Biotechnology Conference. San Francisco, CA; 2010.
Marathe A, Krzyzanski W, Mager D. Numerical validation and properties of a rapid binding approximation of a target-mediated drug disposition pharmacokinetic model. J Pharmacokinet Pharmacodyn. 2009;36:199–219.
ACKNOWLEDGMENTS & DISCLOSURES
I thank Ms. Florence Hourcade-Potelleret for helpful discussions, and I also thank the reviewers for insightful comments.
Author information
Authors and Affiliations
Corresponding author
APPENDIX
APPENDIX
The one-compartment Michaelis-Menten model with a bolus injection and constant total target is a particularly illustrative case for a simplification of the general TMD model under the Qss assumption. We provide here more details of the free drug C that can be expressed using a special mathematical function and the complex M that can be improved over the usual choice. We recommend the use of the improved expression of M (Eq. 46) in modeling.
Inner and Outer Layers
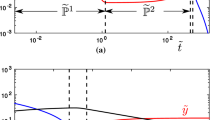
From the terminology of singular perturbation theory, the free drug C (≈ C 0) and complex M given in (29) as a solution to (28) are valid at the initial fast binding time and called the inner layer, but the solution of C and M to (30) and (31) are valid at the later quasi-steady state and called the outer layer. If k e > 0, Eq. 30 for the outer layer can be transformed to a (transcendental) equation after integration
where \( {k_{\text{n}}} = {V_{{\max }}}/{K_{\text{m}}} \) and \( {V_{{\max }}} = {k_{\text{met}}}{R_{\text{tot}}} \). The parameter k n is the maximum nonlinear elimination rate constant for the free drug in the Michaelis-Menten model. The constant \( {G_0} = {G_0}\left( {{C_0}/{K_{\text{m}}},\;{k_{\text{n}}}/{k_{\text{e}}}} \right) \) is equal to the left-hand side of the above equation at t = 0 and thus dependent on C 0/K m and k n/k e. If k e = 0, then V max > 0 (see the assumption of nontrivial TMD models in “Methods”), and the integration of (30) results in the limit of the above equation as k e → 0:
Thus, C is equal to \( {K_{\text{m}}}W\left( {{G_0}{e^{{ - {k_{\text{n}}}t}}}} \right) \) at k e = 0, where W is the Lambert W-function (or omega function), which is the inverse of f (x) = xex. As a generalization of W, if we denote W(x; α) as the inverse of \( f\left( {x;\alpha } \right) = x{\left( {1 + \alpha x} \right)^{{1/\alpha }}} \) then the free drug concentration C in (45) is approximately \( {K_{\text{m}}}W\left( {{G_0}{e^{{\left( { - {k_{\text{e}}} + {k_{\text{n}}}} \right)t}}};\;{k_{\text{e}}}/\left( {{k_{\text{e}}} + {k_{\text{n}}}} \right)} \right) \) for small k e.
Note that a consequence of making the Qss assumption is M (0) = M 0 ≠ 0 if M is the outer layer and given by the first formula in (13), but the limit of the outer layer as t → 0 is the same as the inner layer in (29) as t → ∞. Thus, an improvement to both inner and outer layers as approximations of the complex can be made. With a standard matching technique, a total solution for M can be proposed as the sum of the inner and outer layers minus the overlapping term, which gives
where C is given in (45). Simulation examples in Figs. 5 and 6 show that the improvement corrects the over-estimation of the complex at initial time. In all cases, for small t the improved complex M overlaps completely with that of the general TMD model (plots not shown).
Rights and permissions
About this article
Cite this article
Ma, P. Theoretical Considerations of Target-Mediated Drug Disposition Models: Simplifications and Approximations. Pharm Res 29, 866–882 (2012). https://doi.org/10.1007/s11095-011-0615-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-011-0615-2