Abstract
Background and Objectives
Angiotensin-converting enzyme 2 (ACE2) converts angiotensin II (Ang1-8) to angiotensin 1-7 (Ang1-7), a functional antagonist of Ang1-8, with vasodilatory, antiproliferative, antiangiogenic, and anti-inflammatory properties. In conditions with an unbalanced renin–angiotensin–aldosterone system with elevated Ang1-8, administration of ACE2 has shown promising effects in a variety of animal models. Enhancing ACE2 activity by exogenous administration of ACE2 might also be beneficial in human diseases with pathologically elevated Ang1-8. As a first step we performed a first-in-man study to determine pharmacokinetics, pharmacodynamics, safety, and tolerability of recombinant ACE2 in healthy volunteers.
Methods
Recombinant human ACE2 (rhACE2) was administered intravenously to healthy human subjects in a randomized, double-blind, placebo-controlled, single-dose, dose-escalation study followed by an open-label multiple-dose study. ACE2 concentrations were determined by quantifying ACE2 activity and ACE2 content in plasma samples. Concentrations of the angiotensin system effector peptides Ang1-8, Ang1-7, and Ang1-5 were determined using a liquid chromatography–tandem mass spectrometry method.
Results
Single rhACE2 doses of 100–1,200 μg/kg caused a dose-dependent increase of systemic exposure with biphasic elimination and a dose-independent terminal half-life of 10 h. In all single-dose cohorts, Ang1-8 decreased within 30 min postinfusion, angiotensin 1-7 (Ang1-7) either increased (100 and 200 μg/kg doses), decreased, or remained unchanged (400–1,200 μg/kg doses), whereas angiotensin 1-5 (Ang1-5) transiently increased for all doses investigated. With the exception of the lowest rhACE2 dose, the decrease in Ang1-8 levels lasted for at least 24 h. Repeated dosing (400 μg/kg for 3 or 6 days) caused only minimal accumulation of ACE2, and Ang1-8 levels were suppressed over the whole application period.
Conclusions
Administration of rhACE2 was well tolerated by healthy human subjects. Exposure was dose dependent with a dose-independent terminal elimination half-life in the range of 10 h. Despite marked changes in angiotensin system peptide concentrations, cardiovascular effects were absent, suggesting the presence of effective compensatory mechanisms in healthy volunteers.
Similar content being viewed by others
1 Introduction
The RAS is a central regulator of cardiovascular and renal function, and plays a key role in the pathophysiology of various cardiovascular and renal diseases [1–3]. The effector peptides of the RAS are produced and degraded by a series of enzymatic reactions, which determine effector peptide concentrations in plasma as well as in various tissues. Angiotensin processing is initiated through hydrolysis of the precursor angiotensinogen by the protease renin to generate the biologically inactive decapeptide angiotensin I (Ang1-10) [4, 5]. The peptidase action of ACE converts angiotensin I to the important effector octapeptide angiotensin II (Ang1-8).
Ang1-8 acts as a central mediator of the RAS and is responsible for a variety of physiological effects. Ang1-8 promotes vascular smooth muscle contraction, thereby increasing systemic vascular resistance, initiates sodium reabsorption in the kidney by stimulating aldosterone secretion and is a key regulator of the renal tubulo-glomerular feedback mechanism [6, 7]. Ang1-8 has also been shown to have potent proinflammatory [8–10] and proangiogenic properties [11]. Ang1-8 binds to two distinct receptors (AT-1 and AT-2), with the AT-1 receptor mediating the vasoconstrictive, proliferative and proinflammatory actions of this octapeptide [6]. The function of the AT-2 receptor has not yet been fully clarified.
Recently, ACE2, a homolog of ACE was discovered [12–15]. ACE2 predominantly functions as a monocarboxypeptidase that preferentially hydrolyses between proline and a hydrophobic or basic C-terminal amino acid. The enzymatic reaction most effectively catalyzed by ACE2 is the degradation of Ang1-8 by removing its C-terminal phenylalanine to generate the heptapeptide Ang1-7 [15–17].
In this context, the focus of attention has shifted to the properties of Ang1-7. Ang1-7 functions as an antagonist of Ang1-8, with vasodilatory, antiproliferative, antiangiogenic and anti-inflammatory properties [18]. Ang1-7 effects are mediated by the G-protein coupled Mas-receptor. Ang1-7 also inhibits the activity of the carboxy-terminal domain of ACE, thereby preventing ACE from fully acting on its substrates angiotensin I and bradykinin [19, 20]. Figure 1 gives a simplified overview of the pathways of the RAS and of the functions of Ang1-8, Ang1-7, ACE, and ACE2.
Pharmacological action of ACE2. Similar to ACE, ACE2 can cleave amino acids from angiotensin I (Ang1-10) and angiotensin II (Ang1-8) at the carboxy-terminal. While ACE cleaves two amino acids, ACE2 only cleaves one amino acid. The most important products of ACE2 are therefore Ang1-9 from Ang1-10 and Ang1-7 from Ang1-8. The two products are substrates of ACE and are converted to Ang1-7 and Ang1-5, respectively. To determine the in vivo pharmacological action of ACE2, we quantified Ang1-8, Ang1-7, and Ang1-5 by liquid chromatography–tandem mass spectrometry. ACE angiotensin-converting enzyme, APA aminopeptidase A, APN aminopeptidase N, NO nitric oxide, ROS reactive oxygen species
Modulation of the effector proteins described above can therefore shift the balance in the RAS system from vasoconstrictive, proinflammatory, and growth-promoting conditions to a vasodilatory, anti-inflammatory, and growth-inhibitory state. The balance is maintained by the effects of ACE, Ang1-8, and the AT1 receptor on the one hand, and by ACE2, Ang1-7, and the Mas receptor on the other [21]. Dysregulation of this well-balanced system occurs in several diseases, for example, down-regulation of ACE2 activity in the presence of inflammatory cytokines leading to an accumulation of Ang1-8 [22, 23].
Pathologic effects of chronically elevated Ang1-8 levels have been reported in numerous biological systems, both in experimental as well as clinical settings, [23, 24] and triggered the development of ACE inhibitors, renin inhibitors, and AT1 receptor blockers. Based on the mechanisms described above, the concomitant reduction of Ang1-8 and increase of Ang1-7 levels could have a substantial positive impact in a variety of diseases. Because this double beneficial action could be achieved by the action of ACE2, an enhancement of the activity of this enzyme can be seen as a promising approach for the treatment of diseases and conditions with pathologically enhanced Ang1-8 and/or decreased Ang1-7 levels due to an imbalanced RAS.
In support of this hypothesis, therapeutic effects of rhACE2 were investigated recently in various acute and chronic animal disease models with pathologically elevated Ang1-8 levels or a dysregulated RAS. In ACE2 knockout mice treated with Ang1-8, administration of rhACE2 was able to prevent Ang1-8-associated arterial hypertension, oxidative stress, and tubulo-interstitial fibrosis [25]. Administration of rhACE2 also showed promising effects in murine models of heart hypertrophy, myocardial fibrosis, and cardiac dysfunction [26] and reduced the progression of diabetic nephropathy [27]. Furthermore, rhACE2 inhibited development of liver fibrosis in a bile duct ligation and in a chemically induced liver fibrosis model in mice [28]. Systemic administration of rhACE2 also improved pulmonary blood flow and blood oxygenation in a LPS-induced ARDS model in piglets [29].
ACE2 may thus be developed clinically for the therapy of diseases and syndromes with pathologically elevated Ang1-8. As a first step, we performed a first-in-man dose-escalation, safety and tolerability study assessing the pharmacokinetics and pharmacodynamics of intravenously administered rhACE2 in healthy human subjects.
2 Methods
2.1 Clinical Study
A randomized, double-blind, placebo-controlled, single-dose, dose-escalation study and an open-label, multiple-dose study were performed at the Phase I Research Center, University Hospital Basel, Switzerland. The study was conducted in adherence to International Conference on Harmonization Good Clinical Practice Guideline and in accordance with the principles of the Declaration of Helsinki. The study was approved by the local ethics committee (Ethikkommission Basel, EKBB) and the national regulatory authorities (Swiss Agency for Therapeutic Products, Swissmedic) and registered at clinicaltrials.gov (NCT00886353).
In the dose-escalation part, five cohorts of four subjects each were treated with single doses of rhACE2 (three subjects per cohort) or placebo (one subject per cohort). The starting dose in the first cohort was 100 μg/kg body weight given as an intravenous infusion over 30 min, subsequent cohorts 2–4 were dosed with 200, 400, and 800 μg /kg body weight, respectively. Conduct of the study was monitored by a DSMB. Each dose-escalation event had to be approved by the DSMB based on an interim safety data analysis. Due to the first-in-man application, subjects within cohorts were dosed sequentially; subsequent subjects were only dosed where no DLT was observed within 72 h after each subject in the first cohort and after the first two subjects of cohorts 2–4.
In the open-label part, two cohorts (cohorts 5 and 6) of three subjects each were treated with 400 μg/kg body weight (one dose level lower than the highest tested single dose) per day for three and six consecutive days, respectively. Because no DLT was observed in the highest single-dose (800 μg/kg) cohort, the initial protocol was amended and an additional randomized, double-blind, placebo-controlled, single-dose cohort (cohort 7) was treated with 1,200 μg/kg body weight.
Venous blood samples for pharmacokinetic and pharmacodynamic assays were obtained by an indwelling catheter before (baseline) and after the 30-min study drug infusion (C 0) and 1, 2, 4, 8, and 12 h after study drug administration. For all study drug administrations, a dedicated indwelling catheter on the contralateral arm was used. In the multiple-dose cohorts, samples were collected before (baseline) and after the 30-min study drug infusion and 1, 2, 4, and 8 h after study drug administration on each day of the 3-day cohort and on days 1 and 6 of the 6-day cohort (plus morning samples on days 2–5). In all cohorts, additional samples were collected 24, 48, and 72 h as well as 7 and 14 days after the last study drug administration. To document a potential humoral immune response, plasma samples obtained before and 7 (for multiple-dose cohorts), 14, and 28 days after the last rhACE2 administration were tested using an anti-rhACE2 IgG-specific, IgA-specific, and IgM-specific sandwich ELISA. For pharmacokinetic and immunogenicity analysis, plasma aliquots were collected into heparin tubes, while for pharmacodynamic analyses, aliquots were collected into tubes containing an enzyme inhibitor cocktail composed of phenanthroline, EDTA, beta-mercuri-benzoic-acid, and pepstatin. After centrifugation at 1,800g for 10 min at 4 °C, plasma was stored at −20 °C until analysis. Blood pressure, heart rate, and transcutaneous oxygen saturation were monitored for 24 h (single dose) and for 2 h (multiple-dose cohorts) after study drug application.
2.2 Study Drug
Soluble rhACE2 was produced by Polymun Scientific, Vienna, Austria (contract manufacturer) according to Good Manufacturing Practice guidelines and formulated as a physiological aqueous solution containing 5.2 mg/ml rhACE2 in 100 mM glycine, 150 mM NaCl, and 50 μM ZnCl2 at a pH of 7.5. The study drug was provided to the study site by the sponsor as a sterile, colorless and clear physiological protein solution supplied in sealed glass vials (batch number APN01/0308-A) and stored at ≤−20 °C until use. On study days, the study drug was prepared by two unblinded staff members not involved in the conduct of the study. Vials were thawed at room temperature, the appropriate volume of protein solution based on dose group and body weight was aspirated into a sterile infusion syringe, made up to a final volume of 30 ml with physiological NaCl solution, and labeled with the study subject ID following a written standardized procedure. To ensure correct dosing, vials were weighed before and after aspiration of the study drug and the weight difference was compared with a dose-weight control sheet. Physiological sterile NaCl solution (30 ml) provided by the hospital pharmacy was used as placebo. Infusion syringes filled with 30 ml of clear solution containing either rhACE2 or placebo, labeled with the subject ID, preparation date, and signatures of study personnel responsible for drug preparation were handed over to the blinded study staff for administration as an intravenous infusion at an infusion rate of 1 ml/min.
2.3 Pharmacokinetic Analysis
The ACE2 concentration was determined using two different methods. The first assay quantified enzymatic activity of ACE2 in human heparin plasma samples using MCA-Ala-Pro-Lys(DNP) as substrate. This assay measures the total of endogenous and exogenous ACE2 activity (where contribution of endogenous ACE2 is negligible compared to the amount of exogenous enzyme). ACE2 causes cleavage of the C-terminal Lys residue and removal of the 2,4-dinitrophenyl moiety quenching the fluorescence of 7-methoxycoumarin. The resulting increase in fluorescence was measured photometrically using an Anthos Fluorometer at 320/430 nm. The second assay determined total ACE2 content in plasma using a “sandwich” ELISA. As coating antibody the monoclonal mouse antihuman ACE2 antibody MAB933 (R&D Systems, Minneapolis, MN, USA), as secondary antibody the polyclonal goat antihuman ACE2 antibody AF933 (R&D Systems, Minneapolis, MN, USA), and for detection an antigoat-HRP conjugated antibody and OPD were used. The recombinant expression product was compared to an internal standard. Half-maximal effective concentration (EC50) values were calculated using a four-parameter sigmoidal fit.
Pharmacokinetic parameters for ACE2 activity and content were estimated with Mathcad (PTC®, Needham, MA, USA) using a two-compartment model.
To account for the infusion process for which no data was collected, a linear increase of AUC was assumed and an area defined by the term ½·C (0) × t infusion was added to the AUC obtained by the two-compartment model. Goodness of fit between predicted and measured data was checked by inspection of graphical representation of measured and fitted data and by checking the RMS divided by the initial value (relative RMS).
Immunogenicity of rhACE2 was assessed in plasma samples by a sandwich ELISA using rhACE2 as coating agent and an antihuman IgG, A, M-HRP conjugate as secondary antibody in presence of OPD. Samples were compared to a defined positive control serum raised in Rhesus monkey by active vaccination with rhACE2 formulated as immunogen on Alum-hydrogel.
2.4 Pharmacodynamic Analysis
Concentrations of Ang1-8, Ang1-7, and Ang1-5 in plasma were determined using a liquid chromatography–tandem mass spectrometry (LC-MS/MS) method. Briefly, protease-inhibited plasma samples were spiked with 100 pg/ml stable isotope-labeled internal standards for Ang1-8, Ang1-7, and Ang1-5 (Sigma-Aldrich, St. Louis, MO, USA) and subjected to solid-phase extraction using SEP-Pak C18-Cartridges (500 mg, Waters, Milford, MA, USA) according to the manufacturer’s protocol. Following elution and solvent evaporation, samples were reconstituted in 50 μl of 50 % acetonitrile/0.1 % formic acid and subjected to LC-MS/MS analysis using a reversed phase analytical column [Luna C18(2), 3μ, Phenomenex, Torrance, CA, USA] using a gradient ranging from 10 % acetonitrile/0.1 % formic acid to 70 % acetonitrile/0.1 % formic acid in 9 min. The eluate was analyzed in line using a triple-quadrupole mass spectrometer (API-4000, AB Sciex, Framingham, MA, USA) operated in the MRM mode using dwell times of 25 ms, operating with atmospheric-pressure chemical ionization at a cone voltage of 4,000 V and a source temperature of 300 °C. For each peptide and corresponding internal standards, two different mass transitions were measured. The performance of the method was monitored using quality control samples. Angiotensin peptide concentrations were calculated by relating endogenous peptide signals to internal standard signals provided that integrated signals achieved a signal-to-noise ratio above 10. The quantification limits observed for individual peptides were 1 pg/ml (Ang1-8, Ang1-5) and 2 pg/ml (Ang1-7).
2.5 Statistical Analysis
The SAS/STAT® software package (version 9.1.3, SAS Institute Inc., Cary, NC, USA) was used for statistical analyses. Demographic data, adverse events, and data from physical exams and electrocardiography were analyzed using descriptive statistics stratified by cohort and treatment. Clinical laboratory parameters were assessed by ANOVA or χ² test, as appropriate for the type of data under consideration. Changes in angiotensin peptide concentrations were parametrized by calculating AUEC24 for each peptide and tested with ANOVA and Dunnett’s test for posthoc comparisons.
3 Results
A total of 27 healthy, normal-weight subjects (14 men and 13 women), aged 18 years or older, without history of relevant disease, drug or substance abuse, and with normal findings on physical exam and screening laboratory were included. Due to a randomization error, one subject of the first single-dose cohort had to be replaced and was not included in the statistical analysis.
The plasma concentration–time courses after increasing intravenous rhACE2 doses (see supplementary Figure 1 for treatment schedules) are shown in Fig. 2. An ELISA and a functional assay were used for quantification of ACE2, which yielded almost identical results (Fig. 2a, b). The plasma concentrations were dose dependent. The elimination of rhACE2 was biphasic and could be described by a two-compartment model. The pharmacokinetic variables derived from these measurements are given in Table 1. As expected from the plasma concentrations, the area under the plasma concentration–time curve increased almost linearly with the rhACE2 dose. The terminal elimination half-life was 10.4 ± 4.0 h (mean ± SD) and was not dependent on the rhACE2 dose.
Pharmacokinetics of ACE2 after administration of single and multiple doses. Different doses of rhACE2 (100–1,200 μg/kg) were administered to healthy subjects. ACE2 was quantified using an activity assay (a insert: semi-logarithmic plot) and an ELISA method (b), which gave almost identical results. The kinetic data derived from these curves are given in Table 1. Multiple-dose pharmacokinetics of 400 μg/kg rhACE2 administered daily for 3 or 6 days are shown in c. Regarding trough values, there was only minimal ACE2 accumulation over time. Distribution and elimination of ACE2 did not change during the administration period investigated. ACE angiotensin-converting enzyme, rhACE2 recombinant human angiotensin-converting enzyme 2, ELISA enzyme-linked immunosorbent assay
Daily administration of 400 μg/kg rhACE2 for 3 or 6 days (Fig. 2c) showed no relevant accumulation with time, a finding that is compatible with the elimination half-life of 10 h. The distribution (as reflected by V d and C max) and the elimination of rhACE2 did not change over the entire period of repeated dosing.
The pharmacological activity of rhACE2 was assessed by simultaneously monitoring the concentrations of the substrate (Ang1-8) and the product (Ang1-7) of the reaction catalyzed by ACE2 in addition to a downstream angiotensin metabolite (Ang1-5).
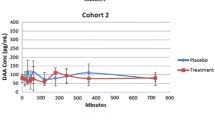
Taking into account the pharmacological activity of ACE2 (as illustrated in Fig. 1), we expected to observe a decrease in Ang1-8 and an increase in Ang1-7 and possibly also in Ang1-5 (depending on the conversion rates of Ang1-8 to Ang1-7 by ACE2 and Ang1-7 to Ang1-5 by ACE). As shown in Fig. 3, after administration of a single dose of 100 μg/kg, the predicted decrease in Ang1-8 and the corresponding increases in Ang1-7 and Ang1-5 were clearly visible. The decrease in Ang1-8 was already detectable 30 min post-rhACE2 infusion, and reached its maximum at a dose of 400 μg/kg. At rhACE2 doses higher than 100 μg/kg, the decrease in Ang1-8 was statistically significant (p < 0.05 for all comparisons vs placebo) and lasted for at least 24 h. The Ang1-7 plasma levels increased after administration of 100 and 200 μg/kg, but remained unchanged or even decreased at higher rhACE2 doses (supplementary Figure S2) for 200 and 800 μg/kg doses (n.s., p > 0.05). The increase in Ang1-5 was observed for every rhACE2 dose investigated (100–1,200 μg/kg), but showed no clear dose dependency in this dose range and did not reach statistical significance (p = 0.065).
Effect of single rhACE2 doses (filled circles, n = 3 per dose group, results for 200 and 800 μg/kg doses are shown in supplementary figure S2) on Ang1-8, Ang1-7, and Ang1-5 compared to levels of placebo-treated subjects (open circles, n = 5). rhACE2 decreased Ang1-8 plasma levels dose dependently, starting at 100 μg/kg and reaching its maximum at 400 μg/kg. For doses of 400 μg/kg or higher, the effect lasted at least for 24 h. The effect of rhACE2 on Ang1-7 was variable. While 100 μg/kg ACE2 increased Ang1-7, doses higher than 400 μg/kg either did not affect or decreased Ang1-7 plasma levels. In contrast to Ang1-7, the administration of rhACE2 was associated with an increase in Ang1-5 for all doses investigated. The effect was not clearly dose dependent and could last up to 48 h after stopping rhACE2 administration. Data are presented as mean and SEM, data from subjects receiving placebo in the single-dose cohorts (n = 5) were pooled. ACE angiotensin-converting enzyme, Ang Angiotensin, rhACE2 recombinant human angiotensin-converting enzyme 2, SEM standard error of mean
Similar to the findings after a single dose, daily rhACE2 administration (400 μg/kg for 3 or 6 days) was associated with a clear decrease in Ang1-8 and an increase in Ang1-5 plasma levels (Fig. 4). Forty-eight hours after stopping the administration of rhACE2, Ang1-8 plasma levels showed an overshoot. They returned to baseline levels after 24 h in all subjects, except one in the 3-day group. Ang1-5 levels returned to baseline levels within 72 h after stopping rhACE2 administration. The trough levels of Ang1-7 were lower or similar compared to plasma levels of untreated control subjects. One of the subjects (3-day group) showed a sharp increase of Ang1-7 and Ang1-5 above physiological levels within 30 min after the last administration of rhACE2 and dropped to levels before rhACE2 administration after 8 h. This was not observed in the other subjects.
Effect of repetitive rhACE2 doses on Ang1-8 (a), Ang1-7 (b), and Ang1-5 (c). Three (black arrows) or six daily doses (grey arrows) of 400 μg/kg rhACE2 were associated with an almost permanent suppression of Ang1-8 plasma levels to subphysiological values lasting for 24 h after the last rhACE2 administration (closed symbols: 3-day administration, n = 3 subjects; open symbols: 6-day administration, n = 3 subjects). Forty-eight hours after the last rhACE2 dose, Ang1-8 had reached higher than physiological levels (dotted line) that remained elevated for the next 24 h in one subject (3-day group), while it dropped to physiological levels within 24 h in all the other subjects. Ang1-7 trough values were generally below the physiological plasma levels and returned to normal levels within 24–48 h. In one subject (3-day group), plasma levels of Ang1-7 and Ang1-5 determined shortly after the last rhACE2 administration reached the supraphysiological range and approached normal levels again within 8 h. This was not observed in the remaining subjects. Ang1-5 trough concentrations were above physiological levels and further increased after rhACE2 administration. After stopping rhACE2 administration, Ang1-5 plasma levels remained elevated for at least 48 h. Ang Angiotensin, rhACE2 recombinant human angiotensin-converting enzyme 2
The administration of rhACE2 was generally well tolerated. Blood pressure and heart rate were not significantly affected by rhACE2 (see supplementary Table 1). Thirty-three adverse events of mild or moderate severity were reported, 26 by subjects treated with rhACE2 and 7 by subjects treated with placebo. None of the reported events was serious. The most often reported events in subjects treated with rhACE2 were diarrhea (4 events in cohort 5) and headache (2 events in cohorts 1 and 7, 1 event in cohorts 4 and 6). None of the subjects experienced a laboratory-related serious adverse event or was discontinued due to a laboratory abnormality. No antibodies to rhACE2 were detected 7 days (multiple-dosage cohorts only), 14, and 28 days after the last dose of rhACE2 using an anti-rhACE2-specific sandwich ELISA.
4 Discussion
In the current study we investigated the pharmacokinetics and pharmacodynamics of a soluble recombinant human ACE2 preparation in healthy subjects. So far, there are no data in the literature about rhACE2 administration in humans, whereas multiple studies have been done using murine model systems [30].
In mice, rhACE2 could be detected in plasma after subcutaneous or intraperitoneal administration, indicating that rhACE2 can be absorbed either by lymphatic vessels or directly across capillary walls [30]. The elimination half-life of rhACE2 was in the range of 8.5 h, a value very close to our findings in humans. In mice, the plasma concentrations of Ang1-8 decreased by approximately 20 % during the subcutaneous administration of rhACE2, which was accompanied by an approximate 20 % increase in the plasma Ang1-7 levels at the two highest doses (1 and 5 mg/kg). In the same study, Ang1-7 plasma levels increased only after previous administration of Ang1-8 [30]. Comparable human data have so far not been available.
In our study, we observed a dose-dependent increase of the exposure to rhACE2, as reflected by the AUC and C max, which reached values of up to 20 μg/ml at the highest dose (1,200 μg/kg) administered. The terminal half-life remained constant at approximately 10 h over the entire dose range. The volume of distribution was also constant at approximately 8 L or 100 mL/kg. This value is larger than the plasma volume, suggesting that ACE2 can reach the extravascular space [31], which is in agreement with the observations in mice described above. The capillary permeability for rhACE2 is limited, however, as expected for a protein of the size of 89.6 kDa [15].
Remarkably, the peak molar ratio in plasma between exogenous rhACE2 and its substrate Ang1-8, exceeded 1,000:1 for every rhACE2 dose administered. Given that under optimized in vitro conditions using an excess amount of substrate, one rhACE2 molecule cleaves and thereby inactivates four molecules of Ang1-8 per second [15], a clear effect on the Ang1-8 plasma concentration could be expected. Indeed, the Ang1-8 plasma concentration decreased dose dependently, reaching the maximal effect after a single dose of 100–400 μg/kg rhACE2. After single rhACE2 doses of 200 μg/kg or higher, Ang1-8 plasma levels remained suppressed for at least 24 h. Accordingly, during daily administration of 400 μg/kg rhACE2 for 3 or 6 days, the Ang1-8 plasma concentration could be kept constantly below physiological levels of 8 pg/ml. In comparison, the administration of 100 μg/kg rhACE2 led only to a short-term suppression of Ang1-8 levels. However, at early time points postadministration, the amplitude of the suppressive effect on Ang1-8 was similar to the effects on Ang1-8 observed with higher doses.
Because Ang1-8 is converted to Ang1-7 by the action of ACE2, an increase in the plasma concentration of Ang1-7 could be expected. Surprisingly, a significant increase was only seen for the two lowest rhACE2 doses (100 and 200 μg/kg), but not for higher doses. The plasma concentration of Ang1-7 depends on multiple factors, such as the overall activity of the RAS (as defined by the input into the RAS via renin) and the relative activities of ACE and ACE2 (see Fig. 1) [32]. Given that Ang1-7 can be converted to Ang1-5 by ACE, the observed increase in Ang1-5 plasma levels after ACE2 administration indirectly confirms the previous formation of Ang1-7 by ACE2. The lack of a consistent increase of the Ang1-7 plasma levels after rhACE2 administration may therefore reflect either different states of basal activity of the RAS (as reflected by the basal Ang1-8 levels) and/or individual variations in ACE activity. Concomitant administration of an ACE inhibitor with rhACE2 could therefore be associated with an increase of Ang1-7 plasma levels. A combination of an ACE inhibitor with rhACE2 may therefore represent a therapeutic option in conditions with renin-independent and ACE-independent Ang1-8 formation and low Ang1-7 plasma levels [33, 34].
In an apparent contradiction to the effects of rhACE2 on the plasma levels of Ang1-8, we observed no effect on blood pressure and pulse rates. This confirms earlier findings that basal vascular resistance in healthy, not sodium-depleted persons is not dependent on Ang1-8 [35, 36]. Similar results were reported in mice treated with rhACE2 [30], supporting our findings and interpretations. The lack of severe adverse reactions associated with rhACE2 in this study confirms the results obtained in preclinical pharmacological and toxicological investigations in rodents [30], piglets [29], and nonhuman primates (data on file), in which much higher doses of rhACE2 (up to 40 mg/kg) have been tested without any tolerability issues. Accordingly, in all of these investigations, the NOAEL corresponded to the highest dose investigated.
In contrast to pharmacological parameters, which can be assessed in animal models, immunogenicity of a recombinant human protein can only be evaluated properly in human clinical trials. rhACE2 did not elicit any immune response following single or repeated dosage in the current study, but further studies with repetitive and longer administration schedules are needed to address this issue properly.
5 Conclusions
The administration of single and multiple doses of rhACE2 was well tolerated by healthy humans and there were no serious adverse events or dose-limiting toxicities. The exposure following rhACE2 administration is dose dependent; the substance has a slightly higher volume of distribution than plasma and is eliminated with a terminal half-life of about 10 h. As expected, rhACE2 efficiently suppresses Ang1-8 plasma levels, whereas Ang1-7 plasma levels are increased only transiently due to rapid conversion to Ang1-5. The absence of effects on blood pressure despite the marked reduction in plasma Ang1-8 shows that the contribution of Ang1-8 to blood pressure regulation is of minor importance in not sodium-depleted healthy persons, underlining the redundant regulation of cardiovascular function in nonpathologic conditions.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- ACE2:
-
Angiotensin-converting enzyme 2 (endogenous protein)
- Ang1-5:
-
Angiotensin 1-5
- Ang1-7:
-
Angiotensin 1-7
- Ang1-8:
-
Angiotensin 1-8
- ANOVA:
-
Analysis of variance
- ARDS:
-
Acute respiratory distress syndrome
- AUC:
-
Area under concentration–time curve
- AUC∞ :
-
Area under concentration–time curve from time zero to infinity
- AUEC24 :
-
Area under effect curve from 0 to 24 hours
- C 0 :
-
Concentration at the end of study drug infusion
- C max :
-
Maximum concentration
- DLT:
-
Dose-limiting toxicity
- DNP:
-
2,4-Dinitrophenyl
- DSMB:
-
Data Safety Monitoring Board
- ELISA:
-
Enzyme-linked immunosorbent assay
- LPS:
-
Lipopolysaccharides
- MCA:
-
(7-Methoxycoumarin-4-yl)acetyl
- NOAEL:
-
No-observed-adverse-effect level
- OPD:
-
o-Phenylenediamine dihydrochloride
- RAS:
-
Renin–angiotensin system
- rhACE2:
-
Recombinant human ACE2
- RMS:
-
Root of mean square error
- t infusion :
-
Duration of study drug infusion
- V d :
-
Volume of distribution
References
Dostal DE, Baker KM. The cardiac renin-angiotensin system: conceptual, or a regulator of cardiac function? Circ Res. 1999;85(7):643–50.
Ito M, Oliverio MI, Mannon PJ, Best CF, Maeda N, Smithies O, et al. Regulation of blood pressure by the type 1A angiotensin II receptor gene. Proc Natl Acad Sci USA. 1995;92(8):3521–5.
Krege JH, John SW, Langenbach LL, Hodgin JB, Hagaman JR, Bachman ES, et al. Male–female differences in fertility and blood pressure in ACE-deficient mice. Nature. 1995;375(6527):146–8.
Hackenthal E, Paul M, Ganten D, Taugner R. Morphology, physiology, and molecular biology of renin secretion. Physiol Rev. 1990;70(4):1067–116.
Tanimoto K, Sugiyama F, Goto Y, Ishida J, Takimoto E, Yagami K, et al. Angiotensinogen-deficient mice with hypotension. J Biol Chem. 1994;269(50):31334–7.
Bernstein KE, Berk BC. The biology of angiotensin II receptors. Am J Kidney Dis. 1993;22(5):745–54.
Turner AJ, Hooper NM. The angiotensin-converting enzyme gene family: genomics and pharmacology. Trends Pharmacol Sci. 2002;23(4):177–83.
Mezzano SA, Ruiz-Ortega M, Egido J. Angiotensin II and renal fibrosis. Hypertension. 2001;38(3 Pt 2):635–8.
Ruiz-Ortega M, Lorenzo O, Ruperez M, Esteban V, Mezzano S, Egido J. Renin-angiotensin system and renal damage: emerging data on angiotensin II as a proinflammatory mediator. Contrib Nephrol. 2001;135:123–37.
Ruiz-Ortega M, Lorenzo O, Ruperez M, Esteban V, Suzuki Y, Mezzano S, et al. Role of the renin-angiotensin system in vascular diseases: expanding the field. Hypertension. 2001;38(6):1382–7.
Herr D, Rodewald M, Fraser HM, Hack G, Konrad R, Kreienberg R, et al. Potential role of Renin-Angiotensin-system for tumor angiogenesis in receptor negative breast cancer. Gynecol Oncol. 2008;109(3):418–25.
Crackower MA, Sarao R, Oudit GY, Yagil C, Kozieradzki I, Scanga SE, et al. Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature. 2002;417(6891):822–8.
Donoghue M, Hsieh F, Baronas E, Godbout K, Gosselin M, Stagliano N, et al. A novel angiotensin-converting enzyme-related carboxypeptidase (ACE2) converts angiotensin I to angiotensin 1-9. Circ Res. 2000;87(5):E1–9.
Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem. 2000;275(43):33238–43.
Vickers C, Hales P, Kaushik V, Dick L, Gavin J, Tang J, et al. Hydrolysis of biological peptides by human angiotensin-converting enzyme-related carboxypeptidase. J Biol Chem. 2002;277(17):14838–43.
Chappell MC. Emerging evidence for a functional angiotensin-converting enzyme 2-angiotensin-(1-7)-MAS receptor axis: more than regulation of blood pressure? Hypertension. 2007;50(4):596–9.
Trask AJ, Averill DB, Ganten D, Chappell MC, Ferrario CM. Primary role of angiotensin-converting enzyme-2 in cardiac production of angiotensin-(1-7) in transgenic Ren-2 hypertensive rats. Am J Physiol Heart Circ Physiol. 2007;292(6):H3019–24.
Lovren F, Pan Y, Quan A, Teoh H, Wang G, Shukla PC, et al. Angiotensin converting enzyme-2 confers endothelial protection and attenuates atherosclerosis. Am J Physiol Heart Circ Physiol. 2008;295(4):H1377–84.
Chappell MC, Allred AJ, Ferrario CM. Pathways of angiotensin-(1-7) metabolism in the kidney. Nephrol Dial Transpl. 2001;16(Suppl 1):22–6.
Yamada K, Iyer SN, Chappell MC, Ganten D, Ferrario CM. Converting enzyme determines plasma clearance of angiotensin-(1-7). Hypertension. 1998;32(3):496–502.
Ferrario CM, Trask AJ, Jessup JA. Advances in biochemical and functional roles of angiotensin-converting enzyme 2 and angiotensin-(1-7) in regulation of cardiovascular function. Am J Physiol Heart Circ Physiol. 2005;289(6):H2281–90.
de Lang A, Osterhaus AD, Haagmans BL. Interferon-gamma and interleukin-4 downregulate expression of the SARS coronavirus receptor ACE2 in Vero E6 cells. Virology. 2006;353(2):474–81.
Hamming I, Cooper ME, Haagmans BL, Hooper NM, Korstanje R, Osterhaus AD, et al. The emerging role of ACE2 in physiology and disease. J Pathol. 2007;212(1):1–11.
Oudit GY, Kassiri Z, Patel MP, Chappell M, Butany J, Backx PH, et al. Angiotensin II-mediated oxidative stress and inflammation mediate the age-dependent cardiomyopathy in ACE2 null mice. Cardiovasc Res. 2007;75(1):29–39.
Zhong J, Guo D, Chen CB, Wang W, Schuster M, Loibner H, et al. Prevention of angiotensin II-mediated renal oxidative stress, inflammation, and fibrosis by angiotensin-converting enzyme 2. Hypertension. 2011;57(2):314–22.
Zhong J, Basu R, Guo D, Chow FL, Byrns S, Schuster M, et al. Angiotensin-converting enzyme 2 suppresses pathological hypertrophy, myocardial fibrosis, and cardiac dysfunction. Circulation. 2010;122(7):717–28, 18 p following 28.
Oudit GY, Liu GC, Zhong J, Basu R, Chow FL, Zhou J, et al. Human recombinant ACE2 reduces the progression of diabetic nephropathy. Diabetes. 2010;59(2):529–38.
Osterreicher CH, Taura K, De Minicis S, Seki E, Penz-Osterreicher M, Kodama Y, et al. Angiotensin-converting-enzyme 2 inhibits liver fibrosis in mice. Hepatology. 2009;50(3):929–38.
Treml B, Neu N, Kleinsasser A, Gritsch C, Finsterwalder T, Geiger R, et al. Recombinant angiotensin-converting enzyme 2 improves pulmonary blood flow and oxygenation in lipopolysaccharide-induced lung injury in piglets. Crit Care Med. 2010;38(2):596–601.
Wysocki J, Ye M, Rodriguez E, Gonzalez-Pacheco FR, Barrios C, Evora K, et al. Targeting the degradation of angiotensin II with recombinant angiotensin-converting enzyme 2: prevention of angiotensin II-dependent hypertension. Hypertension. 2010;55(1):90–8.
Mahmood I, Green MD. Pharmacokinetic and pharmacodynamic considerations in the development of therapeutic proteins. Clin Pharmacokinet. 2005;44(4):331–47.
Iusuf D, Henning RH, van Gilst WH, Roks AJ. Angiotensin-(1-7): pharmacological properties and pharmacotherapeutic perspectives. Eur J Pharmacol. 2008;585(2–3):303–12.
Ahmad S, Simmons T, Varagic J, Moniwa N, Chappell MC, Ferrario CM. Chymase-dependent generation of angiotensin II from angiotensin-(1-12) in human atrial tissue. PloS one. 2011;6(12):e28501.
Park S, Bivona BJ, Kobori H, Seth DM, Chappell MC, Lazartigues E, et al. Major role for ACE-independent intrarenal ANG II formation in type II diabetes. Am J Physiol Ren Physiol. 2010;298(1):F37–48.
Baan J Jr, Chang PC, Vermeij P, Pfaffendorf M, van Zwieten PA. Effects of losartan on vasoconstrictor responses to angiotensin II in the forearm vascular bed of healthy volunteers. Cardiovasc Res. 1996;32(5):973–9.
Newby DE, Masumori S, Johnston NR, Boon NA, Webb DJ. Endogenous angiotensin II contributes to basal peripheral vascular tone in sodium deplete but not sodium replete man. Cardiovasc Res. 1997;36(2):268–75.
Acknowledgments
Manuel Haschke and Manfred Schuster contributed equally to this work. The authors thank Claudia Bläsi, Luisa Baselgia-Jeker, Dietmar Katinger, Thomas Hemetsberger, Bettina Wagner, Evelyne Janzek, Cornelia Schwager, Stefan Stranner, and Robert Weik for their excellent technical assistance.
Disclosures
This study was sponsored by Apeiron Biologics AG. Manfred Schuster, Marko Poglitsch, and Hans Loibner are employees of Apeiron Biologics AG. Manuel Haschke and Stephan Krähenbühl have no financial conflicts to declare (honoraria, speaker fees, etc.) but received funding from Apeiron Biologics AG to conduct the trial. Marc Salzberg received funding from Apeiron Biologics AG for clinical trial administration and monitoring.
Author Contributions
Marc Salzberg, Manfred Schuster, Hans Loibner, Manuel Haschke, and Stephan Krähenbühl designed the research plan.
Manuel Haschke, Marcel Bruggisser, and Stephan Krähenbühl performed the research.
Marko Poglitsch, Manfred Schuster, Hans Loibner, Joseph Penninger, Marc Salzberg, and Manuel Haschke analyzed the data.
Manuel Haschke, Manfred Schuster, Marko Poglitsch, and Stephan Krähenbühl wrote the manuscript.
Marko Poglitsch contributed analytical tools.
Author information
Authors and Affiliations
Corresponding author
Additional information
Clinical Trials Registration Number: NCT00886353.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Haschke, M., Schuster, M., Poglitsch, M. et al. Pharmacokinetics and Pharmacodynamics of Recombinant Human Angiotensin-Converting Enzyme 2 in Healthy Human Subjects. Clin Pharmacokinet 52, 783–792 (2013). https://doi.org/10.1007/s40262-013-0072-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-013-0072-7