Abstract
Objective:
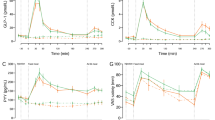
The objective of this study was to quantify hormones that regulate energy and glucose homeostasis to establish possible mechanisms for the greater efficacy of Roux-en-Y gastric bypass (RYGB) compared with laparoscopic adjustable gastric banding (LAGB) in achieving weight loss and improved insulin sensitivity.
Design:
Longitudinal study of patients undergoing LAGB (n=15) and RYGB (n=28) who were studied before surgery and at 2, 12, 26 and 52 weeks afterwards.
Measurements:
Fasting blood samples were drawn at each visit. Postprandial blood samples were also obtained before surgery and at 26 and 52 weeks. Samples were assayed for peptide YY (PYY), ghrelin, glucagon-like peptide-1 (GLP-1), glucose, insulin, leptin, thyrotropic hormone, free T4 and free T3.
Results:
At 1 year there was greater weight loss in RYGB compared with LAGB patients (30 vs 15%), but final body mass index was similar (34 vs 33 kg m−2). At week 52, area under the curve (AUC) for PYY in RYGB subjects was greater than LAGB (P<0.01). GLP-1 levels at 30 min after meal were threefold greater after RYGB compared with LAGB (P<0.001). Conversely, ghrelin AUC increased after LAGB at week 52 (P<0.05) but tended to decrease after RYGB. Fasting glucose, insulin, and leptin and homeostasis model of assessment (HOMA-IR) decreased in both groups over time but were significantly lower at week 52 after RYGB compared with LAGB. The change in leptin correlated significantly with weight loss in LAGB (r=0.86) and RYGB (r=0.77), however, HOMA-IR correlated significantly with weight loss only in LAGB (r=0.78), and not RYGB (r=0.15). There was a significant decrease in free T3 (P<0.01) after RYGB.
Conclusions:
Differences in levels of gut hormones may play a role in promoting greater weight loss and insulin sensitivity after RYGB compared with LAGB, however, weight loss may be limited by decreases in free T3 and leptin.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Freedman DS, Khan LK, Serdula MK, Galuska DA, Dietz WH . Trends and correlates of class 3 obesity in the United States from 1990 through 2000. JAMA 2002; 288: 1758–1761.
Steinbrook R . Surgery for severe obesity. N Engl J Med 2004; 350: 1075–1079.
Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004; 351: 2683–2693.
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004; 292: 1724–1737.
Cummings DE, Overduin J, Foster-Schubert KE . Gastric bypass for obesity: mechanisms of weight loss and diabetes resolution. J Clin Endocrinol Metab 2004; 89: 2608–2615.
Cummings DE, Overduin J, Foster-Schubert KE, Carlson MJ . Role of the bypassed proximal intestine in the anti-diabetic effects of bariatric surgery. Surg Obes Relat Dis 2007; 3: 109–115.
Vincent RP, Ashrafian H, le Roux CW . Mechanisms of disease: the role of gastrointestinal hormones in appetite and obesity. Nat Clin Pract 2008; 5: 268–277.
Wiedmer P, Nogueiras R, Broglio F, D'Alessio D, Tschöp MH . Ghrelin, obesity and diabetes. Nat Clin Pract Endocrinol Metab 2007; 3: 705–712.
Cummings DE, Weigle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP et al. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med 2002; 346: 1623–1630.
Korner J, Bessler M, Inabnet W, Taveras C, Holst JJ . Exaggerated GLP-1 and blunted GIP secretion are associated with gastric bypass but not gastric banding. Surg Obes Relat Dis 2007; 3: 597–601.
Korner J, Inabnet W, Conwell IM, Taveras C, Daud A, Olivero-Rivera L et al. Differential effects of gastric bypass and banding on circulating gut hormone and leptin levels. Obesity 2006; 14: 1553–1561.
Vincent RP, le Roux CW . Changes in gut hormones after bariatric surgery. Clin Endocrinol (Oxf) 2008; 69: 173–179.
Korner J, Bessler M, Cirilo LJ, Conwell IM, Daud A, Restuccia NL et al. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab 2005; 90: 359–365.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Chaikomin R, Doran S, Jones KL, Feinle-Bisset C, O'Donovan D, Rayner CK et al. Initially more rapid small intestinal glucose delivery increases plasma insulin, GIP, and GLP-1 but does not improve overall glycemia in healthy subjects. Am J Physiol Endocrinol Metab 2005; 289: E504–E507.
Borg CM, le Roux CW, Ghatei MA, Bloom SR, Patel AG . Biliopancreatic diversion in rats is associated with intestinal hypertrophy and with increased GLP-1, GLP-2 and PYY levels. Obes Surg 2007; 17: 1193–1198.
Buchan AM, Pederson RA, Koop I, Gourlay RH, Cleator IG . Morphological and functional alterations to a sub-group of regulatory peptides in human pancreas and intestine after jejuno-ileal bypass. Int J Obes Relat Metab Disord 1993; 17: 109–113.
Borg CM, le Roux CW, Ghatei MA, Bloom SR, Patel AG, Aylwin SJ . Progressive rise in gut hormone levels after Roux-en-Y gastric bypass suggests gut adaptation and explains altered satiety. Br J Surg 2006; 93: 210–215.
Kellum JM, Kuemmerle JF, O'Dorisio TM, Rayford P, Martin D, Engle K et al. Gastrointestinal hormone responses to meals before and after gastric bypass and vertical banded gastroplasty. Ann Surg 1990; 211: 763–770.
Laferrère B, Teixeira J, McGinty J, Tran H, Egger JR, Colarusso A et al. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J Clin Endocrinol Metab 2008; 93: 2479–2485.
Muscelli E, Mari A, Casolaro A, Camastra S, Seghieri G, Gastaldelli A et al. Separate impact of obesity and glucose tolerance on the incretin effect in normal subjects and type 2 diabetic patients. Diabetes 2008; 57: 1340–1348.
Verdich C, Toubro S, Buemann B, Lysgard Madsen J, Juul Holst J, Astrup A . The role of postprandial releases of insulin and incretin hormones in meal-induced satiety—effect of obesity and weight reduction. Int J Obes Relat Metab Disord 2001; 25: 1206–1214.
Morinigo R, Vidal J, Lacy AM, Delgado S, Casamitjana R, Gomis R . Circulating peptide YY, weight loss, and glucose homeostasis after gastric bypass surgery in morbidly obese subjects. Ann Surg 2008; 247: 270–275.
le Roux CW, Welbourn R, Werling M, Osborne A, Kokkinos A, Laurenius A et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg 2007; 246: 780–785.
Morinigo R, Casamitjana R, Moize VV, Lacy AM, Delgado S, Gomis R et al. Short-term effects of gastric bypass surgery on circulating ghrelin levels. Obes Res 2004; 12: 1108–1116.
Jeon TY, Lee S, Kim HH, Kim YJ, Son HC, Kim DH et al. Changes in plasma ghrelin concentration immediately after gastrectomy in patients with early gastric cancer. J Clin Endocrinol Metab 2004; 89: 5392–5396.
Williams DL, Grill HJ, Cummings DE, Kaplan JM . Vagotomy dissociates short- and long-term controls of circulating ghrelin. Endocrinology 2003; 144: 5184–5187.
Lee WJ, Lee YC, Ser KH, Chen JC, Chen SC . Improvement of insulin resistance after obesity surgery: a comparison of gastric banding and bypass procedures. Obes Surg 2008; 18: 1119–1125.
Dixon JB, O'Brien PE, Playfair J, Chapman L, Schachter LM, Skinner S et al. Adjustable gastric banding and conventional therapy for type 2 diabetes: a randomized controlled trial. JAMA 2008; 299: 316–323.
Boey D, Sainsbury A, Herzog H . The role of peptide YY in regulating glucose homeostasis. Peptides 2007; 28: 390–395.
Holst JJ . The physiology of glucagon-like peptide 1. Physiol Rev 2007; 87: 1409–1439.
Aulinger B, D'Alessio D . Glucagon-like peptide 1: continued advances, new targets and expanding promise as a model therapeutic. Curr Opin Endocrinol Diabetes Obes 2007; 14: 68–73.
Kok P, Roelfsema F, Langendonk JG, Frolich M, Burggraaf J, Meinders AE et al. High circulating thyrotropin levels in obese women are reduced after body weight loss induced by caloric restriction. J Clin Endocrinol Metab 2005; 90: 4659–4663.
Rosenbaum M, Goldsmith R, Bloomfield D, Magnano A, Weimer L, Heymsfield S et al. Low-dose leptin reverses skeletal muscle, autonomic, and neuroendocrine adaptations to maintenance of reduced weight. J Clin Invest 2005; 115: 3579–3586.
Chan JL, Heist K, DePaoli AM, Veldhuis JD, Mantzoros CS . The role of falling leptin levels in the neuroendocrine and metabolic adaptation to short-term starvation in healthy men. J Clin Invest 2003; 111: 1409–1421.
Carrasco F, Papapietro K, Csendes A, Salazar G, Echenique C, Lisboa C et al. Changes in resting energy expenditure and body composition after weight loss following Roux-en-Y gastric bypass. Obes Surg 2007; 17: 608–616.
Bobbioni-Harsch E, Morel P, Huber O, Assimacopoulos-Jeannet F, Chassot G, Lehmann T et al. Energy economy hampers body weight loss after gastric bypass. J Clin Endocrinol Metab 2000; 85: 4695–4700.
Reinehr T, Isa A, de Sousa G, Dieffenbach R, Andler W . Thyroid hormones and their relation to weight status. Horm Res 2008; 70: 51–57.
Flier JS, Harris M, Hollenberg AN . Leptin, nutrition, and the thyroid: the why, the wherefore, and the wiring. J Clin Invest 2000; 105: 859–861.
Benoit SC, Clegg DJ, Seeley RJ, Woods SC . Insulin and leptin as adiposity signals. Recent Prog Horm Res 2004; 59: 267–285.
Lee M, Wardlaw SL . The central melanocortin system and the regulation of energy balance. Front Biosci 2007; 12: 3994–4010.
Korner J, Punyanita M, Taveras C, McMahon DJ, Kim HJ, Inabnet W et al. Sex differences in visceral adipose tissue post-bariatric surgery compared to matched non-surgical controls. Int J Body Compos Res 2008; 6: 93–99.
Cinti S, de Matteis R, Ceresi E, Pico C, Oliver J, Oliver P et al. Leptin in the human stomach. Gut 2001; 49: 155.
Acknowledgements
We thank the participants in this study. This work was supported by NIH grants DK072011 (to JK) and RR00645 (to the General Clinical Research Center).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Korner, J., Inabnet, W., Febres, G. et al. Prospective study of gut hormone and metabolic changes after adjustable gastric banding and Roux-en-Y gastric bypass. Int J Obes 33, 786–795 (2009). https://doi.org/10.1038/ijo.2009.79
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2009.79
Keywords
This article is cited by
-
Change in Adipokines and Gastrointestinal Hormones After Bariatric Surgery: a Meta-analysis
Obesity Surgery (2023)
-
Strategie di mantenimento del calo ponderale nel paziente con obesità
L'Endocrinologo (2023)
-
Temporospatial shifts in the human gut microbiome and metabolome after gastric bypass surgery
npj Biofilms and Microbiomes (2020)
-
The Fight Against Obesity Escalates: New Drugs on the Horizon and Metabolic Implications
Current Obesity Reports (2020)
-
Sleeve Gastrectomy and Roux-en-Y Gastric Bypass Achieve Similar Early Improvements in Beta-cell Function in Obese Patients with Type 2 Diabetes
Scientific Reports (2019)