Abstract
Cancer cells induce a set of adaptive response pathways to survive in the face of stressors due to inadequate vascularization1. One such adaptive pathway is the unfolded protein (UPR) or endoplasmic reticulum (ER) stress response mediated in part by the ER-localized transmembrane sensor IRE1 (ref. 2) and its substrate XBP1 (ref. 3). Previous studies report UPR activation in various human tumours4,5,6, but the role of XBP1 in cancer progression in mammary epithelial cells is largely unknown. Triple-negative breast cancer (TNBC)—a form of breast cancer in which tumour cells do not express the genes for oestrogen receptor, progesterone receptor and HER2 (also called ERBB2 or NEU)—is a highly aggressive malignancy with limited treatment options7,8. Here we report that XBP1 is activated in TNBC and has a pivotal role in the tumorigenicity and progression of this human breast cancer subtype. In breast cancer cell line models, depletion of XBP1 inhibited tumour growth and tumour relapse and reduced the CD44highCD24low population. Hypoxia-inducing factor 1α (HIF1α) is known to be hyperactivated in TNBCs9,10. Genome-wide mapping of the XBP1 transcriptional regulatory network revealed that XBP1 drives TNBC tumorigenicity by assembling a transcriptional complex with HIF1α that regulates the expression of HIF1α targets via the recruitment of RNA polymerase II. Analysis of independent cohorts of patients with TNBC revealed a specific XBP1 gene expression signature that was highly correlated with HIF1α and hypoxia-driven signatures and that strongly associated with poor prognosis. Our findings reveal a key function for the XBP1 branch of the UPR in TNBC and indicate that targeting this pathway may offer alternative treatment strategies for this aggressive subtype of breast cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011)
Walter, P. & Ron, D. The unfolded protein response: from stress pathway to homeostatic regulation. Science 334, 1081–1086 (2011)
Yoshida, H., Matsui, T., Yamamoto, A., Okada, T. & Mori, K. XBP1 mRNA is induced by ATF6 and spliced by IRE1 in response to ER stress to produce a highly active transcription factor. Cell 107, 881–891 (2001)
Carrasco, D. R. et al. The differentiation and stress response factor XBP-1 drives multiple myeloma pathogenesis. Cancer Cell 11, 349–360 (2007)
De Raedt, T. et al. Exploiting cancer cell vulnerabilities to develop a combination therapy for ras-driven tumors. Cancer Cell 20, 400–413 (2011)
Mahoney, D. J. et al. Virus-tumor interactome screen reveals ER stress response can reprogram resistant cancers for oncolytic virus-triggered caspase-2 cell death. Cancer Cell 20, 443–456 (2011)
Carey, L., Winer, E., Viale, G., Cameron, D. & Gianni, L. Triple-negative breast cancer: disease entity or title of convenience? Nature Rev. Clin. Oncol. 7, 683–692 (2010)
Foulkes, W. D., Smith, I. E. & Reis-Filho, J. S. Triple-negative breast cancer. N. Engl. J. Med. 363, 1938–1948 (2010)
Montagner, M. et al. SHARP1 suppresses breast cancer metastasis by promoting degradation of hypoxia-inducible factors. Nature 487, 380–384 (2012)
The Cancer Genome Atlas Network Comprehensive molecular portraits of human breast tumours. Nature 490, 61–70 (2012)
Idowu, M. O. et al. CD44+/CD24−/low cancer stem/progenitor cells are more abundant in triple-negative invasive breast carcinoma phenotype and are associated with poor outcome. Hum. Pathol. 43, 364–373 (2012)
Lin, Y., Zhong, Y., Guan, H., Zhang, X. & Sun, Q. CD44+/CD24− phenotype contributes to malignant relapse following surgical resection and chemotherapy in patients with invasive ductal carcinoma. J. Exp. Clin. Cancer Res. 31, 59 (2012)
Creighton, C. J. et al. Residual breast cancers after conventional therapy display mesenchymal as well as tumor-initiating features. Proc. Natl Acad. Sci. USA 106, 13820–13825 (2009)
Iliopoulos, D., Hirsch, H. A. & Struhl, K. An epigenetic switch involving NF-κB, Lin28, Let-7 MicroRNA, and IL6 links inflammation to cell transformation. Cell 139, 693–706 (2009)
Iliopoulos, D., Hirsch, H. A., Wang, G. & Struhl, K. Inducible formation of breast cancer stem cells and their dynamic equilibrium with non-stem cancer cells via IL6 secretion. Proc. Natl Acad. Sci. USA 108, 1397–1402 (2011)
Schwab, L. P. et al. Hypoxia inducible factor-1α promotes primary tumor growth and tumor-initiating cell activity in breast cancer. Breast Cancer Res. 14, R6 (2012)
Conley, S. J. et al. Antiangiogenic agents increase breast cancer stem cells via the generation of tumor hypoxia. Proc. Natl Acad. Sci. USA 109, 2784–2789 (2012)
Yang, M. H. et al. Direct regulation of TWIST by HIF-1α promotes metastasis. Nature Cell Biol. 10, 295–305 (2008)
Wouters, B. G. & Koritzinsky, M. Hypoxia signalling through mTOR and the unfolded protein response in cancer. Nature Rev. Cancer 8, 851–864 (2008)
Spiotto, M. T. et al. Imaging the unfolded protein response in primary tumors reveals microenvironments with metabolic variations that predict tumor growth. Cancer Res. 70, 78–88 (2011)
Rody, A. et al. A clinically relevant gene signature in triple negative and basal-like breast cancer. Breast Cancer Res. 13, R97 (2011)
Barnard, G. A. A New Test for 2×2 Tables. Nature 156, 177 (1945)
Barnard, G. A. Significance Tests for 2×2 Tables. Biometrika 34, 123–138 (1947)
Neve, R. M. et al. A collection of breast cancer cell lines for the study of functionally distinct cancer subtypes. Cancer Cell 10, 515–527 (2006)
Chen, X. et al. Integration of external signaling pathways with the core transcriptional network in embryonic stem cells. Cell 133, 1106–1117 (2008)
Li, Q., Brown, J. B., Huang, H. & Bickel, P. J. Measuring reproducibility of high-throughput experiments. Ann. Appl. Stat. 5, 1752–1779 (2011)
Shipitsin, M. et al. Molecular definition of breast tumor heterogeneity. Cancer Cell 11, 259–273 (2007)
Tang, Q. et al. A comprehensive view of nuclear receptor cancer cistromes. Cancer Res. 71, 6940–6947 (2011)
Marotta, L. L. et al. The JAK2/STAT3 signaling pathway is required for growth of CD44+CD24− stem cell-like breast cancer cells in human tumors. J. Clin. Invest. 121, 2723–2735 (2011)
Wang, Y. et al. Gene-expression profiles to predict distant metastasis of lymph-node-negative primary breast cancer. Lancet 365, 671–679 (2005)
Acknowledgements
We thank W. G. Kaelin, A.-H. Lee, F. Martinon, M. N. Wein and X. Li for critical review of the manuscript. We are grateful to A. L. Richardson, H. Xu and J. Wang for advice and discussions. We thank L. A. Paskett, X. Liu, R. Kim and Y. Liu for technical support. This work was supported by the National Institutes of Health (CA112663 and AI32412 to L.H.G.; R01HG004069 to X.S.L.; K99CA175290 to Y.C.), the Leukemia and Lymphoma Society (to X.C.) and the National Natural Science Foundation of China (NSFC31329003 to X.S.L.).
Author information
Authors and Affiliations
Contributions
X.C. and L.H.G. designed the research; X.C., D.I., Q.Z., M.B.G., M.H., E.L., D.Z.H., S.A., B.H., C.T. and M.S. did the experiments; Q.T. and Y.C. performed the bioinformatics analysis; X.S.L. supervised the bioinformatics analysis; M.N., W.L.T., M.B. and S.J.S. contributed to discussions and critical reagents; J.C.C., M.F., M.D.L., H.S. and J.M. contributed to the patient-derived xenograft experiments; X.C. and L.H.G wrote the paper.
Corresponding author
Ethics declarations
Competing interests
L.H.G. holds equity in and is on the corporate board of directors of Bristol-Myers Squibb.
Extended data figures and tables
Extended Data Figure 1 Effect of XBP1 silencing on TNBC cells and UPR.
a, Activation of UPR in different breast cancer cells. Immunoblot of PERK phosphorylation, IRE1α activation (phos-tag SDS–PAGE) and EIF2α phosphorylation in whole-cell lysates, and ATF6α processing (pATF6α) in nuclear extract of basal-like breast cancer cells (1, HCC1937; 2, MDA-MB-231; 3, SUM159; 4, MDA-MB-157; 5, HCC70) and luminal breast cancer cells (6, ZR-75-1; 7, T47D; 8, MCF7). TM, positive control (whole-cell lysates or nuclear extracts from MDA-MB-231 cells treated with 5 μg ml−1 tunicamycin for 6 h). HSP90 was used as loading control for whole-cell lysates, TBP was used as loading control for nuclear extract. b, Transmission electron microscopic analysis of ER in basal-like and luminal breast cancer cell lines. Black arrows indicate the endoplasmic reticulum. All images are at original magnification of 30,000×. Scale bar, 1 μM. c, Quantification of soft agar colony formation and number of invasive cells in untreated and control shRNA or XBP1 shRNA infected breast cancer cells. Experiments were performed in triplicate and data are shown as mean ± s.d. **P < 0.01. d, Quantitative RT–PCR analysis of XBP1 expression in MDA-MB-231 cells infected with lentiviruses encoding doxycycline (dox) inducible shRNAs against XBP1 or scrambled LacZ control, in the presence or absence of doxycycline for 48 h. Data are presented relative to β-actin and shown as mean ± s.d. of technical triplicates. e, f, Knockdown efficiency of total XBP1 (e) and XBP1s (f) in MDA-MB-231-derived xenograft tumour (as in Fig. 1d). Data are presented relative to β-actin. n = 5. g, Bioluminescent images of orthotopic tumours formed by luciferase-expressing MDA-MB-231 cells infected with different lentiviruses. A total of 1.5 × 106 cells were injected into the fourth mammary glands of nude mice. Bioluminescent images were obtained 1 week later and serially after mice were begun on chow containing doxycycline (dox) (day 10). Pictures shown are the day 10 images (before dox) and day 45 images (after dox). h, Effect of XBP1 knockdown on ER stress marker BIP expression in MDA-MB-231-derived xenograft tumours. Quantitative RT–PCR analysis of BIP expression in shCtrl or shXBP1 xenograft tumour. Data are presented relative to β-actin. n = 5. i, Immunoblot of IRE1α activation (phos-tag SDS–PAGE) and PERK phosphorylation in whole-cell lysates; ATF6α processing and ATF4 expression in nuclear extracts of two shCtrl or shXBP1 xenograft tumours. HSP90 was used as loading control for whole-cell lysates; TBP was used as loading control for nuclear extract. j, k, Tumour growth of untreated or control shRNA, or XBP1 shRNA treated MDA-MB-436 (j) or HBL-100 cells (k) in nude mice. Data are shown as mean ± s.d. of biological replicates (n = 3). **P < 0.01. Tx: treatment with shRNA. l, Kaplan–Meier tumour-free survival curve of mice from Fig. 1f. m, Tumour growth (mean ± s.e.m.) of BCM-2147 tumours as in Fig. 1f (Scr siRNA, n = 7; XBP1 siRNA, n = 2).
Extended Data Figure 2 Effect of XBP1 on tumour relapse and CD44highCD24low cells.
a, Tumour growth of MDA-MB-231 cells untreated or treated with paclitaxel (20 mg kg−1), or paclitaxel + control shRNA, or paclitaxel + XBP1 shRNA in nude mice. TX, treatment with paclitaxel or paclitaxel + shRNA. Data are shown as mean ± s.d. of biological replicates (n = 5). b, Number of mammospheres per 1,000 cells generated from day 20 xenograft tumours under different treatments as indicated under normoxic or hypoxic condition (0.1% O2). Data are shown as mean ± s.d. of biological replicates (n = 3). Asterisk denotes significantly different from paclitaxel + shCtrl control in each treatment; *P < 0.05, **P < 0.01. c, Effect of XBP1 knockdown on cell death in hypoxic regions (assessed by CA9 and cleaved caspase 3 staining) or accumulation of CD44highCD24low cells (assessed by CD44 staining). Immunohistochemical staining of CA9 and cleaved caspase 3 (consecutive sections) showed that cell death was not induced in hypoxic region in XBP1 knockdown tumours. Immunohistochemical staining of CD44 showed significant reduction of CD44 expression in XBP1 knockdown tumours. All tumour sections are from MDA-MB-231-derived xenograft with different treatment as indicated. d, Knockdown efficiency of XBP1 in MCF10A-ER-Src cells. Data are shown as mean ± s.d. of technical triplicates. e, Left panel: flow cytometry analysis of CD44 and CD24 expression of tamoxifen-treated (36 h) MCF10A ER-Src cells infected with control shRNA or XBP1 shRNA encoding lentivirus. Right panel: percentage of CD44highCD24low cells in tamoxifen (4-OH-tamoxifen)-treated MCF10A-ER-Src cells infected with control shRNA or XBP1 shRNA encoding lentivirus. Experiments were performed in triplicate and data are shown as mean ± s.d. *P < 0.05. f, Number of mammospheres per 1,000 cells generated by tamoxifen-treated MCF10A ER-Src cells uninfected, or infected with control shRNA or XBP1 shRNA encoding lentivirus. Experiments were performed in triplicate and data are shown as mean ± s.d. g, Cell viability assay (Cell-titer Glo) on CD44highCD24low or CD44lowCD24high cells isolated from tamoxifen-treated MCF10A-ER-Src cells infected with control shRNA or XBP1 shRNA encoding lentivirus (72 h after infection). Data were normalized to the control (cell infected with shCtrl). Experiments were performed in triplicate and data are shown as mean ± s.d. h, Cleaved caspase 3 ELISA assays on CD44highCD24low or CD44lowCD24high cells isolated from tamoxifen-treated MCF10A-ER-Src cells infected with control shRNA or XBP1 shRNA encoding lentivirus (72 h after infection). Experiments were performed in triplicate and data are shown as mean ± s.d.
Extended Data Figure 3 Effect of XBP1 on CD44highCD24low cells.
a, UPR markers are upregulated in CD44highCD24low cells. Quantitative RT–PCR analysis of UPR markers BIP, CHOP, ERDJ4, HERP and MBTPS1 in CD44lowCD24high cells and CD44highCD24low cells sorted from two TNBC patients. Data are shown as mean ± s.d. of technical triplicates. *P < 0.05, **P < 0.01. b, XBP1s overexpression in CD44lowCD24high cells generates mammosphere-forming ability. Number of mammospheres per 1,000 cells generated by sorted CD44lowCD24high cells transduced with empty vector or XBP1s expressing retrovirus. Experiments were performed in triplicate and data are shown as mean ± s.d. c, CD44lowCD24high cells overexpressing XBP1s are more resistant to chemotherapy. MTT (3-[4,5-dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide) assay was performed to measure the dose–response curves of CD44lowCD24high cells or CD44lowCD24high cells expressing XBP1s treated with doxorubicin. Experiments were performed in triplicate and data are shown as mean ± s.d. *P < 0.05, **P < 0.01. d, 1,000 or 100 CD44lowCD24high cells sorted from transformed MCF10A ER-Src cells or CD44lowCD24high cells overexpressing XBP1s were injected into NOD/SCID/Il2rγ−/− mice and the incidence of tumours was monitored. e, Ten CD44lowCD24high cells sorted from two human patients with TNBC or CD44lowCD24high cells overexpressing XBP1s were injected into NOD/SCID/Il2rγ−/− mice and the incidence of tumours was monitored.
Extended Data Figure 4 HIF1α is a co-regulator of XBP1.
a, Identification of XBP1 motif in MDA-MB-231 ChIP-seq data set. Matrices predicted by the de novo motif-discovery algorithm Seqpos. P < 1.08 × 10−30. b, Induction of XBP1 splicing by hypoxia. RT–PCR analysis of the ratio of XBP1s to total XBP1 in MDA-MB-231 cells cultured under normoxic condition or hypoxic condition (0.1% O2) for 24 h. Data are shown as mean ± s.d. of technical triplicates. **P < 0.01. c, Induction of XBP1 splicing by glucose deprivation. RT–PCR analysis of the ratio of XBP1s to total XBP1 in MDA-MB-231 cells cultured in normal medium or glucose-free medium for 24 h or 48 h. Data are shown as mean ± s.d. of technical triplicates. *P < 0.05. d, Induction of XBP1 splicing by oxidative stress. RT–PCR analysis of the ratio of XBP1s to total XBP1 in MDA-MB-231 cells untreated or treated with different doses of H2O2 for 1 h, 4 h or 24 h. Data are shown as mean ± s.d. of technical triplicates. e, Western blotting analysis of XBP1s expression in nuclear extract of MDA-MB-231 cells cultured under normoxia or hypoxia (0.1% O2) and glucose-free condition for 16 h. Lamin B was used as loading control. f, Venn diagram showing the overlap between XBP1 targets in MDA-MB-231 breast cancer cells cultured under normoxic conditions (untreated) or hypoxia and glucose deprivation conditions (treated). g, Motif enrichment analysis in the XBP1 binding sites in untreated or stressed (0.1% O2 and glucose deprivation: HG) MDA-MB-231, Hs578T or T47D cells. The 1-kb region surrounding the summit of the XBP1 peak is equally divided into 50 bins. The average HIF1α motif occurrence over top 1,000 XBP1 peaks in each bin is plotted. The corresponding P values of each condition are listed as follows: M231_Un, 7.78 × 10−20; M231_HG, <1.08 × 10−30; Hs578T_HG, <1.08 × 10−30; T47D_HG, 6.14 × 10−6. h, Flag-tagged HIF1α and XBP1s were co-expressed in 293T cells, and the cells were treated in 0.1% O2 for 16 h. Co-immunoprecipitation was performed with M2 anti-Flag antibody. Western blot was carried out with anti-XBP1s antibody, anti-Flag antibody or anti-HIF1α antibody. Empty vector was used as control. i, Nuclear extracts from Hs578T cells treated with tunicamycin (1 μg ml−1, 6 h) in 0.1% O2 (16 h) were subjected to co-immunoprecipitation with anti-HIF1α antibody or rabbit IgG. Western blot was carried out with anti-XBP1s antibody or anti-HIF1α antibody. j, HA-tagged HIF2α and XBP1s were co-expressed in 293T cells, and the cells were treated in 0.1% O2 for 16 h. Co-immunoprecipitation was performed with anti-HA antibody. Western blot was carried out with anti-XBP1s antibody or anti-HA antibody. Empty vector was used as control. k, Localization of XBP1s and HIF1α in MDA-MB-231 cells. Western blotting analysis of XBP1s and HIF1α expression in cytosolic extracts and nuclear extracts of MDA-MB-231 cells cultured under 0.1% O2 condition for 24 h. HSP90 and TBP were used as control. l, XBP1u is not expressed in MDA-MB-231 cells. Western blotting analysis of XBP1u in MDA-MB-231 cells untreated or treated with 1 μM or 10 μM MG132 for 4 h. HSP90 was used as loading control. m, Schematic diagram of full-length and truncated forms of XBP1s protein. n, A GST pull-down assay was performed using GST-tagged XBP1s proteins and 293T cell lysates overexpressing HA-tagged HIF1α. Western blotting was performed with an anti-HA antibody. Lower panel: Coomassie blue staining of GST-tagged different truncated forms of XBP1s proteins.
Extended Data Figure 5 XBP1 and HIF1α co-occupy HIF1α targets.
a, Track view of XBP1 ChIP-seq density profile (two biological replicates) on HIF1α target genes. b, XBP1 and HIF1α co-bind to DDIT4, VEGFA and PDK1 promoters under hypoxic conditions. A ChIP assay was performed using anti-XBP1 or anti-HIF1α antibody to detect enriched fragments. GST antibody was used as mock ChIP control. c, XBP1 and HIF1α co-bind to JMJD1A and JMJD2C promoters under hypoxic conditions. Upper panel: schematic diagram of the primer locations across the JMJD2C or JMJD1A promoter. Grey boxes indicate exon. A ChIP assay was performed using anti-XBP1 polyclonal antibody or anti-HIF1α polyclonal antibody to detect enriched fragments. Fold enrichment is the relative abundance of DNA fragments at the amplified region over a control amplified region. GST antibody was used as mock ChIP control. d, XBP1s and HIF1α co-occupy JMJD1A, DDIT4, NDRG1, PDK1 and VEGFA promoters. A ChIP-re-ChIP assay was performed using the anti-XBP1s antibody first (X). The eluants were then subjected to a second ChIP assay using an anti-HIF1α antibody (XH) or a control IgG antibody (XC). All ChIP data (b–d) are shown as mean ± s.d. of technical triplicates. Results show a representative of two independent experiments. *P < 0.05; **P < 0.01. e, HIF1α, but not XBP1s, binds to a probe in Twist promoter in 293T cells. DNA pull-down assay was used to analyse the binding of XBP1s or HIF1α on a probe in Twist promoter. The nuclear extracts of 293T cells overexpressing XBP1s or Flag–HIF1α was incubated with the wild-type probe and immunoblot analysis was performed with anti-XBP1s or anti-Flag antibody. f, XBP1s binds to Twist promoter in MDA-MB-231 cells under 0.1% O2. The nuclear extract of MDA-MB-231 cells cultured under 0.1% O2 for 24 h was incubated with the wild-type or mutant probe (HIF1α consensus sequence was mutated) and immunoblot analysis was performed with anti-XBP1s or anti-HIF1α antibody. The lower panel shows the sequence of the probes used. g, 3×HRE reporter was co-transfected with XBP1s expression plasmid or empty vector into MDA-MB-231 cells and luciferase activity measured. Experiments were performed in triplicate and data are shown as mean ± s.d. **P < 0.01. h, RT–PCR analysis of XBP1 expression as in g. Data are shown as mean ± s.d. of technical triplicates.
Extended Data Figure 6 XBP1 regulates HIF1α targets.
a, Plot from GSEA showing enrichment of the HIF1α-mediated hypoxia response pathway in XBP1-upregulated genes. b, Quantitative RT–PCR analysis of VEGFA, PDK1, GLUT1 and DDIT4 expression after knockdown of XBP1 in MDA-MB-231 under both normoxic or hypoxic conditions. c, Quantitative RT–PCR analysis of VEGFA, PDK1, GLUT1, MCT4, JMJD1A and XBP1 expression after knockdown of XBP1 in Hs578T cells treated with 0.1% O2 for 24 h. Results are presented relative to β-actin expression. Experiments were performed in triplicate and data are shown as mean ± s.d. *P < 0.05, **P < 0.01. d, Plot from GSEA showing no enrichment of the HIF1α-mediated hypoxia response pathway in XBP1-regulated genes in T47D cells (P = 0.1684). e–k, Cooperative binding of XBP1 and HIF1α on common targets. e, Immunoblotting analysis of control MDA-MB-231 cell lysates and XBP1 knockdown lysates (treated with 0.1% O2 for 24 h) were performed using anti-HIF1α or anti-HSP90 antibody. f, g, Chromatin extracts from control MDA-MB-231 cells or XBP1 knockdown MDA-MB-231 cells (treated with 0.1% O2 for 24 h) were subjected to ChIP using anti-XBP1s antibody (f), or anti-RNA polymerase II antibody (g). The primers used to detect ChIP-enriched DNA were the peak pair of primers in JMJD1A, DDIT4, NDRG1, PDK1 and VEGFA promoters (Supplementary Table 3). Primers in the β-actin region were used as control. h, i, Chromatin extracts from control MDA-MB-231 cells or HIF1α knockdown MDA-MB-231 cells (treated with 0.1% O2 for 24 h) were subjected to ChIP using anti-HIF1α antibody (h), or anti-RNA polymerase II antibody (i). j, k, Chromatin extracts from control MDA-MB-231 cells or XBP1 knockdown MDA-MB-231 cells (treated with 1% O2 for 24h) were subjected to ChIP using anti-HIF1α antibody (j), and anti-XBP1s antibody (k). All ChIP data (f–k) are shown as mean ± s.d. of technical triplicates. Results show a representative of two independent experiments. *P < 0.05; **P < 0.01. l, Quantitative RT–PCR analysis of VEGFA, PDK1, GLUT1 and JMJD1A after knockdown of XBP1 in MDA-MB-231 cells treated with 1% O2 for 24 h. Results are presented relative to β-actin expression. Data are shown as mean ± s.d. of technical triplicates. *P < 0.05, **P < 0.01.
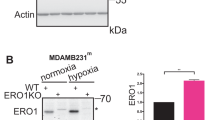
Extended Data Figure 7 Overexpression of constitutively activated HIF1α rescues XBP1 knockdown phenotype.
a, Immunoblotting analysis of cell lysates of MDA-MB-231 cells infected with retrovirus encoding control vector or HA–HIF1α dPA was performed using anti-HA or anti-actin antibody. b, XBP1 splicing is not affected by HIF1α or HIF2α activation. RT–PCR analysis of the ratio of XBP1s to total XBP1 in MDA-MB-231 cells expressing control vector, HA–HIF1α dPA or HA–HIF2α dPA. Expression of HA–HIF1α dPA is shown in a and expression of HIF2α is shown in the right panel. c, XBP1 splicing is not affected by HIF1α or HIF2α depletion. RT–PCR analysis of the ratio of XBP1s to total XBP1 in MDA-MB-231 cells infected with control, shHIF1α or shHIF2α lentivirus. Knockdown efficiency of HIF1α or HIF2α is shown in the middle and right panels. d, e, Expression of constitutively activated HIF1α doesn’t affect XBP1 expression (d), but restores HIF1α targets expression (e). RT–PCR analysis of XBP1 total (d), XBP1s (d) and VEGFA, PDK1, DDIT4 (e) in control shRNA (shCtrl), XBP1 shRNA (shXBP1), or XBP1 shRNA plus constitutively activated HIF1α (shXBP1+HIF1α dPA) infected MDA-MB-231 cells. Data (b–e) are shown as mean ± s.d. of technical triplicates. *P < 0.05, **P < 0.01. f, Quantification of soft agar colony formation in control shRNA (shCtrl), XBP1 shRNA (shXBP1), or XBP1 shRNA plus constitutively activated HIF1α (shXBP1 + HIF1α dPA) infected MDA-MB-231, MDA-MB-468, or MDA-MB-157 cells. Experiments were performed in triplicate and data are shown as mean ± s.d. **P < 0.01. g, Quantification of mammosphere formation in control shRNA (shCtrl), XBP1 shRNA (shXBP1), or XBP1 shRNA plus constitutively activated HIF1α (shXBP1+HIF1α dPA) infected MDA-MB-231 cells. Experiments were performed in triplicate and data are shown as mean ± s.d. **P < 0.01. h, CD31 immunostaining of tumours formed by MDA-MB-231 cells infected with control shRNA (shCtrl), XBP1 shRNA (shXBP1) or XBP1 shRNA plus constitutively activated HIF1α (shXBP1+HIF1α dPA). i, Silencing of HIF1α inhibits the XBP1s-sustained mammosphere-forming ability. Quantification of mammosphere formation in MCF10A cells expressing control vector, XBP1s, XBP1s plus control shRNA or XBP1s plus HIF1α shRNA. Experiments were performed in triplicate and data are shown as mean ± s.d. **P < 0.01.
Extended Data Figure 8 Schema depicting the interaction of XBP1 and HIF1α in TNBC.
XBP1 and HIF1α cooperatively regulate HIF1α targets in TNBC. In the setting of a tumour microenvironment, hypoxia further induces XBP1 activation; active XBP1s in turn interacts with HIF1α to stimulate and augment the transactivation of HIF1 target genes that promote cancer progression.
Extended Data Figure 9 Correlation of XBP1 with HIF1α in patients with TNBC.
a, b, Expression of XBP1 signature is highly correlated with two publicly available hypoxia-driven signatures in TNBC patients (a), but not in ER+ breast cancer patients (b). The scatter plots of XBP1 and two publicly available HIF1α signatures (left panel, HIF1α pathway; right panel, hypoxia via HIF1α pathway) across different tumours were drawn for TNBC (a) and ER+ breast cancer patients (b), respectively. The corresponding Pearson’s correlation coefficient (r) between XBP1 and HIF1α signature is shown. c, d, Kaplan–Meier graphs demonstrating no significant association of the expression of the XBP1 signature (red line) (c) or HIF signature (d) with relapse-free survival in oestrogen-receptor-positive breast cancer patients. The log-rank test P values are shown.
Extended Data Figure 10 Role of XBP1 in luminal breast cancer.
a, XBP1 splicing is induced by hypoxia and glucose deprivation in luminal cancer cells. RT–PCR of XBP1 splicing in T47D and SKBR3 cells under different treatments for 24 h. XBP1u, unspliced XBP1; XBP1s, spliced XBP1. Hypoxia: 0.1% O2. b, Left panel: quantification of soft agar colony formation in untreated and control shRNA or XBP1 shRNA infected breast cancer cells. Experiments were performed in triplicate and data are shown as mean ± s.d. **P < 0.01. Right panel: effect of XBP1 depletion on soft agar colony formation in luminal versus basal cell lines. Percentages of soft agar colonies formed from cells infected with XBP1 shRNA lentivirus relative to the same cell line infected with shCtrl lentivirus (set as 100%) are presented. 5 cell lines in each group (as in left panel) and data are shown as mean ± s.d. c, Tumour growth (mean ± s.d.) of ZR-75-1 cells treated with control shRNA (n = 4), paclitaxel (20 mg kg−1) + control shRNA (n = 4), XBP1 shRNA (n = 4) or paclitaxel + XBP1 shRNA (n = 3) in nude mice. TX, treatment with shRNA or paclitaxel + shRNA. Asterisk denotes shXBP1-treated tumours significantly different from shCtrl-treated tumours; P < 0.05. d, Number of mammospheres per 1,000 cells generated by control shRNA or XBP1 shRNA-encoding lentivirus infected T47D or SKBR3 breast cancer cell lines cultured under normoxia or hypoxia and glucose deprivation conditions (treated). Experiments were performed in triplicate and data are shown as mean ± s.d. e, Venn diagram showing the overlap between XBP1 targets in MDA-MB-231, Hs578T cells and T47D cells cultured under hypoxia and glucose deprivation conditions. f, XBP1s overexpression is not capable of converting a luminal phenotype to basal phenotype. RT–PCR analysis of luminal marker (CK8, CK18, CK19 and E-cadherin) and basal marker (CK5, CK14, p63, fibronectin and vimentin) expression in luminal breast cancer cells (MCF7 or T47D) infected with lentivirus encoding empty vector or XBP1s. Data are shown as mean ± s.d. of technical triplicates.
Supplementary information
Supplementary Table 1
This file contains a Supplementary Table listing genes of the XBP1 gene signature. (XLS 33 kb)
Supplementary Table 2
This file contains a Supplementary Table listing the clinical information of TNBC patient cohorts. (XLS 280 kb)
Supplementary Table 3
This file contains a Supplementary Table listing the ChIP primer sequences used in this study. (XLS 23 kb)
Rights and permissions
About this article
Cite this article
Chen, X., Iliopoulos, D., Zhang, Q. et al. XBP1 promotes triple-negative breast cancer by controlling the HIF1α pathway. Nature 508, 103–107 (2014). https://doi.org/10.1038/nature13119
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nature13119
This article is cited by
-
Emerging mechanisms of the unfolded protein response in therapeutic resistance: from chemotherapy to Immunotherapy
Cell Communication and Signaling (2024)
-
Targeting the IRE1α-XBP1s axis confers selective vulnerability in hepatocellular carcinoma with activated Wnt signaling
Oncogene (2024)
-
HIF1α-dependent hypoxia response in myeloid cells requires IRE1α
Journal of Neuroinflammation (2023)
-
RRM2 and CDC6 are novel effectors of XBP1-mediated endocrine resistance and predictive markers of tamoxifen sensitivity
BMC Cancer (2023)
-
NIR diagnostic imaging of triple-negative breast cancer and its lymph node metastasis for high-efficiency hypoxia-activated multimodal therapy
Journal of Nanobiotechnology (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.