Abstract
Understanding the cellular mechanisms of tumour growth is key for designing rational anticancer treatment. Here we used genetic lineage tracing to quantify cell behaviour during neoplastic transformation in a model of oesophageal carcinogenesis. We found that cell behaviour was convergent across premalignant tumours, which contained a single proliferating cell population. The rate of cell division was not significantly different in the lesions and the surrounding epithelium. However, dividing tumour cells had a uniform, small bias in cell fate so that, on average, slightly more dividing than non-dividing daughter cells were generated at each round of cell division. In invasive cancers induced by KrasG12D expression, dividing cell fate became more strongly biased towards producing dividing over non-dividing cells in a subset of clones. These observations argue that agents that restore the balance of cell fate may prove effective in checking tumour growth, whereas those targeting cycling cells may show little selectivity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Accession codes
References
Pierce, G. B. & Wallace, C. Differentiation of malignant to benign cells. Cancer Res. 31, 127–134 (1971).
Torre, L. A. et al. Global cancer statistics, 2012. CA Cancer J. Clin. 65, 87–108 (2015).
Shapiro, J. et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 16, 1090–1098 (2015).
Taylor, P. R., Abnet, C. C. & Dawsey, S. M. Squamous dysplasia—the precursor lesion for esophageal squamous cell carcinoma. Cancer Epidemiol. Biomarkers Prev. 22, 540–552 (2013).
Wang, G. Q. et al. Histological precursors of oesophageal squamous cell carcinoma: results from a 13 year prospective follow up study in a high risk population. Gut 54, 187–192 (2005).
Rubio, C. A., Liu, F. S., Chejfec, G. & Sveander, M. The induction of esophageal tumors in mice: dose and time dependency. In Vivo 1, 35–38 (1987).
Hecht, S. S. Tobacco smoke carcinogens and lung cancer. J. Natl Canc. Inst. 91, 1194–1210 (1999).
Reuber, M. D. Histopathology of preneoplastic and neoplastic lesions of the esophagus in BUF rats ingesting diethylnitrosamine. J. Natl Canc. Inst. 58, 313–321 (1977).
Liu, K. et al. Sox2 cooperates with inflammation-mediated Stat3 activation in the malignant transformation of foregut basal progenitor cells. Cell Stem Cell 12, 304–315 (2013).
Stairs, D. B. et al. Deletion of p120-catenin results in a tumor microenvironment with inflammation and cancer that establishes it as a tumor suppressor gene. Cancer Cell 19, 470–483 (2011).
Opitz, O. G. et al. A mouse model of human oral-esophageal cancer. J. Clin. Invest. 110, 761–769 (2002).
Ohkoshi, A., Suzuki, T., Ono, M., Kobayashi, T. & Yamamoto, M. Roles of Keap1-Nrf2 system in upper aerodigestive tract carcinogenesis. Cancer Prev. Res. 6, 149–159 (2012).
Doupe, D. P. et al. A single progenitor population switches behavior to maintain and repair esophageal epithelium. Science 337, 1091–1093 (2012).
Alcolea, M. P. & Jones, P. H. Tracking cells in their native habitat: lineage tracing in epithelial neoplasia. Nat. Rev. Cancer 13, 161–171 (2013).
Alcolea, M. P. et al. Differentiation imbalance in single oesophageal progenitor cells causes clonal immortalization and field change. Nat. Cell Biol. 16, 615–622 (2014).
Vermeulen, L. et al. Defining stem cell dynamics in models of intestinal tumor initiation. Science 342, 995–998 (2013).
Roshan, A. et al. Human keratinocytes have two interconvertible modes of proliferation. Nat. Cell Biol. 18, 145–156 (2016).
Alcolea, M. P. & Jones, P. H. Cell competition: winning out by losing notch. Cell Cycle 14, 9–17 (2015).
Abel, E. L., Angel, J. M., Kiguchi, K. & DiGiovanni, J. Multi-stage chemical carcinogenesis in mouse skin: fundamentals and applications. Nat. Protoc. 4, 1350–1362 (2009).
Wilhelm, S. M. et al. Preclinical overview of sorafenib, a multikinase inhibitor that targets both Raf and VEGF and PDGF receptor tyrosine kinase signaling. Mol. Cancer Ther. 7, 3129–3140 (2008).
Arnault, J. P. et al. Keratoacanthomas and squamous cell carcinomas in patients receiving sorafenib. J. Clin. Oncol. 27, e59–e61 (2009).
Schneider, T. C. et al. (Secondary) solid tumors in thyroid cancer patients treated with the multi-kinase inhibitor sorafenib may present diagnostic challenges. BMC Cancer 16, 31 (2016).
Takahashi, K. & Coulombe, P. A. Defining a region of the human keratin 6a gene that confers inducible expression in stratified epithelia of transgenic mice. J. Biol. Chem. 272, 11979–11985 (1997).
Wilson, J. B., Weinberg, W., Johnson, R., Yuspa, S. & Levine, A. J. Expression of the BNLF-1 oncogene of Epstein-Barr virus in the skin of transgenic mice induces hyperplasia and aberrant expression of keratin 6. Cell 61, 1315–1327 (1990).
Hobbs, R. P. et al. Keratin-dependent regulation of Aire and gene expression in skin tumor keratinocytes. Nat. Genet. 47, 933–938 (2015).
Hanahan, D. & Folkman, J. Patterns and emerging mechanisms of the angiogenic switch during tumorigenesis. Cell 86, 353–364 (1996).
Schoppmann, S. F. et al. Lymphangiogenesis and lymphovascular invasion diminishes prognosis in esophageal cancer. Surgery 153, 526–534 (2013).
Kubota, Y. et al. The onset of angiogenesis in a multistep process of esophageal squamous cell carcinoma. Front. Biosci. 14, 3872–3878 (2009).
Zheng, W., Aspelund, A. & Alitalo, K. Lymphangiogenic factors, mechanisms, and applications. J. Clin. Invest. 124, 878–887 (2014).
Kitadai, Y. et al. Clinicopathological significance of vascular endothelial growth factor (VEGF)-C in human esophageal squamous cell carcinomas. Int. J. Cancer 93, 662–666 (2001).
Jensen, M. A., Wilkinson, J. E. & Krainer, A. R. Splicing factor SRSF6 promotes hyperplasia of sensitized skin. Nat. Struct. Mol. Biol. 21, 189–197 (2014).
Nowell, P. C. The clonal evolution of tumor cell populations. Science 194, 23–28 (1976).
Martincorena, I. & Campbell, P. J. Somatic mutation in cancer and normal cells. Science 349, 1483–1489 (2015).
Winton, D. J., Blount, M. A. & Ponder, B. A. Polyclonal origin of mouse skin papillomas. Br. J. Cancer 60, 59–63 (1989).
Ross-Innes, C. S. et al. Whole-genome sequencing provides new insights into the clonal architecture of Barrett’s esophagus and esophageal adenocarcinoma. Nat. Genet. 47, 1038–1046 (2015).
Parsons, B. L. Many different tumor types have polyclonal tumor origin: Evidence and implications. Mutat. Res. 659, 232–247 (2008).
Schepers, A. G. et al. Lineage tracing reveals Lgr5+ stem cell activity in mouse intestinal adenomas. Science 337, 730–735 (2012).
Maddipati, R. & Stanger, B. Z. Pancreatic cancer metastases harbor evidence of polyclonality. Cancer Discov. 5, 1086–1097 (2015).
Shin, K. et al. Cellular origin of bladder neoplasia and tissue dynamics of its progression to invasive carcinoma. Nat. Cell Biol. 16, 469–478 (2014).
Snippert, H. J. et al. Intestinal crypt homeostasis results from neutral competition between symmetrically dividing Lgr5 stem cells. Cell 143, 134–144 (2010).
Kemp, R. et al. Elimination of background recombination: somatic induction of Cre by combined transcriptional regulation and hormone binding affinity. Nucleic Acids Res. 32, e92 (2004).
Gao, Y. B. et al. Genetic landscape of esophageal squamous cell carcinoma. Nat. Genet. 46, 1097–1102 (2014).
Song, Y. et al. Identification of genomic alterations in oesophageal squamous cell cancer. Nature 509, 91–95 (2014).
Lin, D. C. et al. Genomic and molecular characterization of esophageal squamous cell carcinoma. Nat. Genet. 46, 467–473 (2014).
Arnault, J. P. et al. Skin tumors induced by sorafenib; paradoxic RAS-RAF pathway activation and oncogenic mutations of HRAS, TP53, and TGFBR1. Clin. Cancer Res. 18, 263–272 (2012).
Jackson, E. L. et al. Analysis of lung tumor initiation and progression using conditional expression of oncogenic K-ras. Genes Dev. 15, 3243–3248 (2001).
Wilson, A. et al. Hematopoietic stem cells reversibly switch from dormancy to self-renewal during homeostasis and repair. Cell 135, 1118–1129 (2008).
Mascre, G. et al. Distinct contribution of stem and progenitor cells to epidermal maintenance. Nature 489, 257–262 (2012).
Tumbar, T. et al. Defining the epithelial stem cell niche in skin. Science 303, 359–363 (2004).
Hochedlinger, K., Yamada, Y., Beard, C. & Jaenisch, R. Ectopic expression of Oct-4 blocks progenitor-cell differentiation and causes dysplasia in epithelial tissues. Cell 121, 465–477 (2005).
Harris, M. E. et al. Regulation of histone mRNA in the unperturbed cell cycle: evidence suggesting control at two posttranscriptional steps. Mol. Cell. Biol. 11, 2416–2424 (1991).
Whitfield, M. L. et al. Stem-loop binding protein, the protein that binds the 3′ end of histone mRNA, is cell cycle regulated by both translational and posttranslational mechanisms. Mol. Cell. Biol. 20, 4188–4198 (2000).
Salic, A. & Mitchison, T. J. A chemical method for fast and sensitive detection of DNA synthesis in vivo. Proc. Natl Acad. Sci. USA 105, 2415–2420 (2008).
Tabassum, D. P. & Polyak, K. Tumorigenesis: it takes a village. Nat. Rev. Cancer 15, 473–483 (2015).
Kreso, A. & Dick, J. E. Evolution of the cancer stem cell model. Cell Stem Cell 14, 275–291 (2014).
Meacham, C. E. & Morrison, S. J. Tumour heterogeneity and cancer cell plasticity. Nature 501, 328–337 (2013).
Clayton, E. et al. A single type of progenitor cell maintains normal epidermis. Nature 446, 185–189 (2007).
Doupe, D. P., Klein, A. M., Simons, B. D. & Jones, P. H. The ordered architecture of murine ear epidermis is maintained by progenitor cells with random fate. Dev. Cell 18, 317–323 (2010).
Sharma, A. et al. Mutant V599EB-Raf regulates growth and vascular development of malignant melanoma tumors. Cancer Res. 65, 2412–2421 (2005).
Peyre, E. et al. A lateral belt of cortical LGN and NuMA guides mitotic spindle movements and planar division in neuroepithelial cells. J. Cell Biol. 193, 141–154 (2011).
Du, P., Kibbe, W. A. & Lin, S. M. lumi: a pipeline for processing Illumina microarray. Bioinformatics 24, 1547–1548 (2008).
Ritchie, M. E. et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 43, e47 (2015).
Falcon, S. & Gentleman, R. Using GOstats to test gene lists for GO term association. Bioinformatics 23, 257–258 (2007).
Szklarczyk, D. et al. STRING v10: protein–protein interaction networks, integrated over the tree of life. Nucleic Acids Res. 43, D447–D452 (2014).
Acknowledgements
We thank S. Malhotra, Consultant Upper GI Pathologist at Addenbrookes Hospital Cambridge for assistance with histopathology. This work was funded by a Cancer Research UK Programme Grant (C609/A17257) to P.H.J., a Medical Research Council Grant-in-Aid and core support at the Wellcome Trust Sanger Institute. P.G. was funded by a DFG Research Fellowship and an EPSRC Critical Mass Grant. B.D.S. acknowledges the support of the Wellcome Trust (grant number 098357/Z/12/Z) and the core funding to the Gurdon Institute by the Wellcome Trust and Cancer Research UK.
Author information
Authors and Affiliations
Contributions
J.F. designed and performed experiments, analysed data and wrote the manuscript, P.G. carried out quantitative analysis and wrote the manuscript, B.D.S. carried out quantitative analysis and wrote the manuscript, P.H.J. initiated and supervised the project and wrote the manuscript, T.N. performed bioinformatic analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Transgenic assays to track cell behaviour used in this study.
(a) cre-mediated recombination allows for conditional expression of a heritable genetic label. cre recombinase activity is subject to dual regulation, at the transcriptional level and at the level of nuclear translocation. Expression of a cre recombinase-mutant oestrogen receptor fusion protein (creERT) from a drug-regulated promoter is achieved upon treatment with β-napthoflavone (BNF). Upon binding of tamoxifen (Tam), the fusion protein changes conformation and translocates to the nucleus, where it mediates recombination of the loxP sites, thus activating reporter (b,c) or mutant (d) alleles. (b) Genetic lineage tracing in AhcreERTRosa26flConfetti/wt mice. The multicolour confetti reporter allele encodes four fluorescent proteins. Different cre-mediated inversion and excision recombination events result in the heritable expression of one of the four fluorescent proteins depicted, green fluorescent protein (GFP), yellow fluorescent protein (YFP), red fluorescent protein (RFP) or cyan fluorescent protein (CFP). Once recombination is achieved, the reporter will be expressed in all the progeny of the marked cell, which continue to proliferate and differentiate, generating clusters of labelled cells termed clones. (c) Genetic lineage tracing in AhcreERTRosa26flYFP/wt mice. Induction of cre recombination results in excision of a stop cassette and heritable expression of the single colour yellow fluorescent protein (YFP) reporter. (d) Induction of the oncogenic LSL-KrasG12D mutant allele. cre-mediated recombination results in the excision of a STOP cassette and heritable expression of the Kras mutant (red star). (e) For quantification of the cell division rate, animals carrying a reverse tetracycline-controlled transactivator (rtTA-M2) and a HIST1H2BJ/EGFP fusion protein (HGFP) expressed from a tetracycline responsive promoter element were used. Doxycycline (dox) treatment in these animals results in nuclear labelling of all basal cells in the oesophageal epithelium with HGFP. Upon withdrawal of dox, HGFP transcription and translation ceases and the protein is diluted by cell division (see Supplementary Note 2.1).
Supplementary Figure 2 Effect of Sorafenib on oesophageal epithelium.
(a–c) Proliferation following Sorafenib treatment. (a) Protocol. Animals were treated with Sorafenib or vehicle only (Control) for 10 days and injected with EdU (purple arrow) 1 h before being culled. (b,c) Box plots showing dose response to Sorafenib of percentage of EdU + (b) and Ki67 + (c) basal cells in epithelial wholemounts. Values are % positive cells/field in random fields of view from duplicate animals at each time point. Number of fields sampled in b was 0 mg and 1 mg, 12 fields, 10 mg, 9 fields, 50 mg 11 fields, 100 mg 10 fields, and in c 0 mg, 10 fields, 1 mg and 10 mg, 9 fields, 50 mg 8 fields, 100 mg 10 fields. Box indicates 25th and 75th centiles, centre line is median, whiskers indicate range. (d–h) Characterization of epithelium after 28 days Sorafenib treatment. (d) Protocol. (e) Confocal image of epithelial cryosection stained for Cryosection stained for P-AKT (Ser473, green) and basal marker ITGA6 (white) and DAPI (blue). Scale bar, 50 μm. Arrow, cells positive for P-AKT. Image representative of sections from 3 animals/group. (f) Mean percentage of basal cells staining positive for P-AKT (∗P = 0.011 by two tailed t-test, n = 4 animals/group). (g) Typical confocal images of epithelial cryosections stained for basal keratinocyte marker KRT14 (green), suprabasal marker KRT4 (magenta), basal marker ITGA6 (white) and DAPI (blue). Scale bar, 50 μm. Arrow, cells double positive for KRT4 and KRT14 (inset). (h) Mean percentage of cells staining positive for activated Caspase 3, n = 3 animals per group. See Supplementary Table 4 for source data for b,c and f.
Supplementary Figure 3 Further characterization of HGD lesions.
(a) Effect of DEN and Sorafenib treatment on differentiation. Confocal image of cyrosection from lesion stained for terminal differentiation marker FLG (green), KRT4 (magenta) and basal cell marker KRT14 (white). Scale bar, 200 μm. (b) Confocal image of cryosection stained for keratinocyte stress induced protein KRT17 (green) and basal cell marker ITGA6 (white). Scale bar, 200 μm. Images a,b are representative of 3 lesions. (c)Immune infiltrate in stromal wholemount stained for pan leukocyte marker CD45 (green) and KRT14 (magenta) marking lesion, Scale bar, 100 μm. Image representative of at least 3 tumours. (d–g) Clonal origin of HGD lesions. (d) Protocol. In AhcreERTRosa26flYFP/wt mice YFP was induced and animals then treated with DEN and Sorafenib to induce lesions. Possible outcomes are shown. Lesions derived from a single cell would be either unlabelled or completely labelled, while the presence of multiple labelled and/or unlabelled areas indicates multiple cells of origin. (e) Oblique view of 3D rendered confocal Z stack of typical lesion, dotted white line indicates lesion edge, YFP is green, KRT14 magenta. Scale bar, 200 μm. Projected confocal optical sections of typical lesion, YFP is green, KRT14 is magenta, ITGA6 is white. Scale bar, 100 μm. Images in e are representative of 14 lesions. (f) YFP + cell clusters per lesion (n = 18 lesions from 6 animals). Line indicates mean. (g) Area of YFP + clusters (n = 51 clusters from 6 lesions). Line indicates mean. See Supplementary Table 4 for source data for f and g.
Supplementary Figure 4 Characterisation of squamous cell carcinomas.
(a,b) Cryosections stained for KRT14 (a) or LOR (b, green). KRT4 is magenta, ITGA6 white and DAPI blue. Scale bars, 200 μm and 100 μm, respectively. Images are representative of 3 tumours. (c) ErbB signaling pathway based on Kegg pathway analysis (http://www.genome.jp/kegg/kegg3a.html). The colour indicates the logarithmic fold changes of gene expression between SCC and HGD, boxes are gene products, + p protein interaction via phosphorylation, solid line direct protein-protein interaction, dashed line: indirect interaction, arrows indicate activation, T ended lines inhibition.
Supplementary Figure 5 Cell dynamics in Sorafenib treated epithelium.
(a) Mean cell generations (completed cell divisions 24 h post dox withdrawal) inferred from HGFP dilution in >300 cells/animal (3 animals/time point or 4 at 72 h). Data error bars are given as s.e.m. of log HGFP fluorescence, due to mouse-to-mouse variation (Supplementary Note 2.1). Dashed line: least-squares linear regression with slope of 1.00 ± 0.03 (s.e.m.)/day, that approximates mean cell division rate (Supplementary Note 2.1). (b) Distribution of cell generations, 48 h (black, 3 animals) and 72 h (purple, 4 animals) after Dox withdrawal. Relative measured HGFP fluorescence/cell, f, and cell generations, n, assigned by n = log2(f(24 h)/f) (Supplementary Note 2.1). Error bars: s.e.m. (c–f) Lineage tracing in Sorafenib treated animals (Fig. 5d–f). (c) Clone size distributions (CSD), 12 days after induction (green bars, 233 clones). Points, model predictions by best fit parameters, bars, s.d. of predicted values). (d,e) Basal cells/clone. Points, experimental data, lines, model predictions, blue shading, s.d. of prediction (Supplementary Note 2.2). (d) Comparison between stochastic (black) and synchronous cell division models (orange), using parameters fitted for Sorafenib-treated tissue (Supplementary Note 2.2). (e) Vehicle compared with model predictions from normal oesophagus, 12 days after induction (n = 232 clones). (f) Representativeness of clones in Sorafenib treated mice, Protocol as Fig. 5d. Mean % EdU + cells inside and outside YFP + clones (difference not significant, P = 0.47 by two-tailed t-test, n = 3 mice per group). (g–j) Lineage tracing in Sorafenib treated AhcreERTR26flEYFP/wt animals 21 days after induction. (g) Protocol. labelling was induced (green arrow) after 28 days of Sorafenib treatment, which continued for a further 21 days. (h,i) , basal h and total i cells/clone in Sorafenib-treated animals, 21 days post labelling. Points, experimental data (n = 112 clones from 4 animals), lines, model predictions for best fit parameters, blue area s.d. of predictions (Supplementary Note 2.2). (j) CSD 21 days after induction (112 clones), compared with predictions based on parameter estimates from 12 day experiment. Green bars, experimental data; points, model predictions; bars, s.d. of predicted values. (k–q) Validation of model (k) Protocol to test prediction that 50% of EdU + cells stratify in 24 h (Supplementary Note 2.2 and Supplementary Table 5). (l) Typical lateral projection of epithelium; EdU (green), ITGA6 (white). Scale bar, 20 μm. (m) Proportion of suprabasal (sb)/total EdU + cells, values are means from 3 fields-of-view/animal ∗∗∗P < 0.0001 by two-tailed t-test, n = 3 mice. (n–q) Protocol (n) to test if predicted increase in asymmetric divisions alters mitotic orientation (o) Typical mitoses stained with PCNT (green); basal marker ITGA6 (white) and DAPI (blue). Scale bar, 10 μm. (p–q) Spindle angle relative to basement membrane (0°) in Sorafenib-treated (p, n = 30 mitoses) and control animals (q, n = 41 mitoses). ∗∗∗P < 0.0001 by Kolmogorov-Smirnov test. See Supplementary Table 4 for source data for a–f,h–j,m,p and q.
Supplementary Figure 6 Cell dynamics in HGD lesions.
(a) Box plots of HGFP fluorescence intensity in HGD from at time points shown (see Fig. 6f for protocol). Box indicates 25th and 75th percentiles, line median and whiskers range. n = 100 cells at 0 h, 277 cells at 24 h, 361 cells at 48 h, 600 cells at 72 h. (b,c) Distribution of cell generations at 48 (black) and 72 (purple) hours, after dox withdrawal in HGD (b) and adjacent epithelium (c) (see Fig. 6f and Supplementary Note 2.3). Error bars are standard deviation. (b) In HGD, at 48 h (n = 4 animals), and 72 h (n = 6 animals). (c) In adjacent epithelium (n = 3 animals both time points). (d) Cell division rates per day inferred from HGFP dilution. Errors are s.e.m. (e–h) Lineage tracing in DEN and Sorafenib treated animals. (e) Clone size distribution 22 days after induction of YFP (protocol shown in Fig. 7a). Points are experimental data (n = 68 clones) with clone size binned in intervals of 5 cells per clone. Lines are model predictions by best-fit parameters and blue area shows standard deviation of the prediction (see Supplementary Note 2.3). (f) Representativeness of clones in HGD. In protocol shown in Fig. 7a animals received a pulse of EdU 1 h prior to being culled. Mean percentage EdU labelling within clones (total 1126 cells) and the entire lesion (total 9792 cells), error bars s.e.m. P = 0.40 by Mann Whitney test (n = 56 clones). (g) Clone size distribution (n = 106 clones) in epithelium adjacent to HGD 13 days after induction of YFP, distinguishing basal and suprabasal cells per clone. Height of bars/points indicates the frequency of clones with the given number of basal and suprabasal cells, as indicated on the axes. Green bars are experimental data, points model predictions by best fit parameters, error bars standard deviations of predicted values (see Supplementary Note 2.3). (h) Cell dynamics in HGD in AhcreERTRosa26flConfetti/wt mice, see Fig. 7e–g. Clone size distributions 21 days after induction. Points are experimental data (n = 101 clones from 5 animals), lines model fits and blue area indicates standard deviation (see Supplementary Note 2.3). Data are binned in intervals of 5 cells per clone. See Supplementary Table 4 for source data for a–c and e–h.
Supplementary Figure 7 Cell dynamics in Ras- driven SCCs.
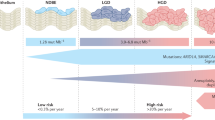
(a,b) Representativeness of clones in SCC in AhcreERTRosa26flYFP/wtKrasflG12D/wt animals, induced after DEN exposure and before Sorafenib treatment as shown in Fig. 8a. (a) Mean percentage EdU + cells, 1 h after labelling, in whole tumours and YFP + clones within them, n.s. P = 0.69 by Kolmogorov-Smirnov test, n = 23 clones from 3 tumours. (b) Mean percentage Ki67 + cells in whole tumours and clones within them, n.s. P = 0.34 by two tailed t-test, n = 12 clones from 4 tumours. (c,d) Clone size distributions 56 days after induction. Points are experimental data, lines model predictions and blue area shows standard deviation of the prediction. Data is binned in intervals of 10 cells per clone (c) and 100 cells per clone (d), respectively. (c) Clones <200 cells (n = 25 clones), 56 days after induction, shown with model prediction derived from HGD lesions (see Fig. 7d). (d) Rescaled clone size distribution for clones > 200 cells (n = 16 clones), at 56 days after induction, together with theoretical prediction (exponential function), see Supplementary Note 2.4 for discussion. (e) Cryosection of SCC stained for proliferation marker Ki67 (green) and basal cell marker ITGA6 (white). Scale bar, 100 μm and 50 μm, respectively. Image is representative of 4 tumours. (f) Summary: proliferating cell fate in oesophageal carcinogenesis. In histologically normal epithelium, even after exposure to nitrosamine and Sorafenib, cell production (green arrow) equals cell loss (red arrow). Proliferating cell fate is balanced, generating equal proportions of dividing and non-dividing cells on average. In tumours, an excess of dividing cells is generated locally. This is achieved through a small bias in cell fate towards producing proliferating progeny, Δ, and a reduction in the rate of cell loss relative to cell production.
Supplementary information
Supplementary Information
Supplementary Information (PDF 1791 kb)
Supplementary Table 2
Supplementary Information (XLSX 9 kb)
Supplementary Table 3
Supplementary Information (XLSX 15 kb)
Supplementary Table 4
Supplementary Information (XLSX 23 kb)
Supplementary Table 5
Supplementary Information (XLSX 198 kb)
Supplementary Table 6
Supplementary Information (XLSX 10 kb)
Supplementary Table 7
Supplementary Information (XLSX 10 kb)
Supplementary Table 8
Supplementary Information (XLSX 49 kb)
Rights and permissions
About this article
Cite this article
Frede, J., Greulich, P., Nagy, T. et al. A single dividing cell population with imbalanced fate drives oesophageal tumour growth. Nat Cell Biol 18, 967–978 (2016). https://doi.org/10.1038/ncb3400
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncb3400
This article is cited by
-
Enhancement of TKI sensitivity in lung adenocarcinoma through m6A-dependent translational repression of Wnt signaling by circ-FBXW7
Molecular Cancer (2023)
-
Notch1 mutations drive clonal expansion in normal esophageal epithelium but impair tumor growth
Nature Genetics (2023)
-
Regenerative medicine: current research and perspective in pediatric surgery
Pediatric Surgery International (2023)
-
p53 mutation in normal esophagus promotes multiple stages of carcinogenesis but is constrained by clonal competition
Nature Communications (2022)
-
Pyrimethamine inhibits cell growth by inducing cell senescence and boosting CD8+ T-cell mediated cytotoxicity in colorectal cancer
Molecular Biology Reports (2022)