Abstract
Marfan syndrome (MFS) is a heritable connective tissue disorder caused by mutations in FBN1, which encodes the extracellular matrix protein fibrillin-1. To investigate the pathogenesis of aortic aneurysms in MFS, we generated a vascular model derived from human induced pluripotent stem cells (MFS-hiPSCs). Our MFS-hiPSC-derived smooth muscle cells (SMCs) recapitulated the pathology seen in Marfan aortas, including defects in fibrillin-1 accumulation, extracellular matrix degradation, transforming growth factor-β (TGF-β) signaling, contraction and apoptosis; abnormalities were corrected by CRISPR-based editing of the FBN1 mutation. TGF-β inhibition rescued abnormalities in fibrillin-1 accumulation and matrix metalloproteinase expression. However, only the noncanonical p38 pathway regulated SMC apoptosis, a pathological mechanism also governed by Krüppel-like factor 4 (KLF4). This model has enabled us to dissect the molecular mechanisms of MFS, identify novel targets for treatment (such as p38 and KLF4) and provided an innovative human platform for the testing of new drugs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
McKusick, V.A. The cardiovascular aspects of Marfan's syndrome: a heritable disorder of connective tissue. Circulation 11, 321–342 (1955).
Pyeritz, R.E. & McKusick, V.A. The Marfan syndrome: diagnosis and management. N. Engl. J. Med. 300, 772–777 (1979).
Dietz, H.C., Loeys, B., Carta, L. & Ramirez, F. Recent progress towards a molecular understanding of Marfan syndrome. Am. J. Med. Genet. C. Semin. Med. Genet. 139C, 4–9 (2005).
Robinson, P.N. et al. The molecular genetics of Marfan syndrome and related disorders. J. Med. Genet. 43, 769–787 (2006).
Milewicz, D.M., Dietz, H.C. & Miller, D.C. Treatment of aortic disease in patients with Marfan syndrome. Circulation 111, e150–e157 (2005).
Dietz, H.C. et al. Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 352, 337–339 (1991).
Pereira, L. et al. Targetting of the gene encoding fibrillin-1 recapitulates the vascular aspect of Marfan syndrome. Nat. Genet. 17, 218–222 (1997).
ten Dijke, P. & Arthur, H.M. Extracellular control of TGFβ signalling in vascular development and disease. Nat. Rev. Mol. Cell Biol. 8, 857–869 (2007).
Kaartinen, V. & Warburton, D. Fibrillin controls TGF-β activation. Nat. Genet. 33, 331–332 (2003).
Ramirez, F. & Dietz, H.C. Marfan syndrome: from molecular pathogenesis to clinical treatment. Curr. Opin. Genet. Dev. 17, 252–258 (2007).
Habashi, J.P. et al. Losartan, an AT1 antagonist, prevents aortic aneurysm in a mouse model of Marfan syndrome. Science 312, 117–121 (2006).
Neptune, E.R. et al. Dysregulation of TGF-β activation contributes to pathogenesis in Marfan syndrome. Nat. Genet. 33, 407–411 (2003).
Jones, J.A., Spinale, F.G. & Ikonomidis, J.S. Transforming growth factor-β signaling in thoracic aortic aneurysm development: a paradox in pathogenesis. J. Vasc. Res. 46, 119–137 (2009).
Doyle, J.J., Gerber, E.E. & Dietz, H.C. Matrix-dependent perturbation of TGFβ signaling and disease. FEBS Lett. 586, 2003–2015 (2012).
Cook, J.R. et al. Dimorphic effects of transforming growth factor-β signaling during aortic aneurysm progression in mice suggest a combinatorial therapy for Marfan syndrome. Arterioscler. Thromb. Vasc. Biol. 35, 911–917 (2015).
Lacro, R.V. et al. Atenolol versus losartan in children and young adults with Marfan's syndrome. N. Engl. J. Med. 371, 2061–2071 (2014).
Pereira, L. et al. Pathogenetic sequence for aneurysm revealed in mice underexpressing fibrillin-1. Proc. Natl. Acad. Sci. USA 96, 3819–3823 (1999).
Cook, J.R. et al. Abnormal muscle mechanosignaling triggers cardiomyopathy in mice with Marfan syndrome. J. Clin. Invest. 124, 1329–1339 (2014).
Holm, T.M. et al. Noncanonical TGFβ signaling contributes to aortic aneurysm progression in Marfan syndrome mice. Science 332, 358–361 (2011).
Takahashi, K. et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131, 861–872 (2007).
Cheung, C., Bernardo, A.S., Pedersen, R.A. & Sinha, S. Directed differentiation of embryonic origin-specific vascular smooth muscle subtypes from human pluripotent stem cells. Nat. Protoc. 9, 929–938 (2014).
Schrijver, I., Liu, W., Brenn, T., Furthmayr, H. & Francke, U. Cysteine substitutions in epidermal growth factor-like domains of fibrillin-1: distinct effects on biochemical and clinical phenotypes. Am. J. Hum. Genet. 65, 1007–1020 (1999).
Faivre, L. et al. Effect of mutation type and location on clinical outcome in 1,013 probands with Marfan syndrome or related phenotypes and FBN1 mutations: an international study. Am. J. Hum. Genet. 81, 454–466 (2007).
Attanasio, M. et al. FBN1 mutation screening of patients with Marfan syndrome and related disorders: detection of 46 novel FBN1 mutations. Clin. Genet. 74, 39–46 (2008).
Cheung, C., Bernardo, A.S., Trotter, M.W.B., Pedersen, R.A. & Sinha, S. Generation of human vascular smooth muscle subtypes provides insight into embryological origin-dependent disease susceptibility. Nat. Biotechnol. 30, 165–173 (2012).
Vallier, L. et al. Early cell fate decisions of human embryonic stem cells and mouse epiblast stem cells are controlled by the same signalling pathways. PLoS One 4, e6082 (2009).
Laiho, M., Saksela, O. & Keski-Oja, J. Transforming growth factor-beta induction of type-1 plasminogen activator inhibitor. Pericellular deposition and sensitivity to exogenous urokinase. J. Biol. Chem. 262, 17467–17474 (1987).
Owens, G.K., Kumar, M.S. & Wamhoff, B.R. Molecular regulation of vascular smooth muscle cell differentiation in development and disease. Physiol. Rev. 84, 767–801 (2004).
Syyong, H.T., Chung, A.W.Y. & van Breemen, C. Marfan syndrome decreases Ca2+ wave frequency and vasoconstriction in murine mesenteric resistance arteries without changing underlying mechanisms. J. Vasc. Res. 48, 150–162 (2011).
Syyong, H.T., Chung, A.W.Y., Yang, H.H.C. & van Breemen, C. Dysfunction of endothelial and smooth muscle cells in small arteries of a mouse model of Marfan syndrome. Br. J. Pharmacol. 158, 1597–1608 (2009).
Keane, M.G. & Pyeritz, R.E. Medical management of Marfan syndrome. Circulation 117, 2802–2813 (2008).
Chung, A.W.Y. et al. Loss of elastic fiber integrity and reduction of vascular smooth muscle contraction resulting from the upregulated activities of matrix metalloproteinase-2 and -9 in the thoracic aortic aneurysm in Marfan syndrome. Circ. Res. 101, 512–522 (2007).
Crosas-Molist, E. et al. Vascular smooth muscle cell phenotypic changes in patients with Marfan syndrome. Arterioscler. Thromb. Vasc. Biol. 35, 960–972 (2015).
Meilhac, O. et al. Pericellular plasmin induces smooth muscle cell anoikis. FASEB J. 17, 1301–1303 (2003).
Quarto, N. et al. Skeletogenic phenotype of human Marfan embryonic stem cells faithfully phenocopied by patient-specific induced-pluripotent stem cells. Proc. Natl. Acad. Sci. USA 109, 215–220 (2012).
Majesky, M.W. Developmental basis of vascular smooth muscle diversity. Arterioscler. Thromb. Vasc. Biol. 27, 1248–1258 (2007).
Sinha, S., Iyer, D. & Granata, A. Embryonic origins of human vascular smooth muscle cells: implications for in vitro modeling and clinical application. Cell. Mol. Life Sci. 71, 2271–2288 (2014).
Goumans, M.-J., Liu, Z. & ten Dijke, P. TGF-β signaling in vascular biology and dysfunction. Cell Res. 19, 116–127 (2009).
Loeys, B.L. et al. A syndrome of altered cardiovascular, craniofacial, neurocognitive and skeletal development caused by mutations in TGFBR1 or TGFBR2. Nat. Genet. 37, 275–281 (2005).
Doyle, A.J. et al. Mutations in the TGF-β repressor SKI cause Shprintzen-Goldberg syndrome with aortic aneurysm. Nat. Genet. 44, 1249–1254 (2012).
van de Laar, I.M.B.H. et al. Mutations in SMAD3 cause a syndromic form of aortic aneurysms and dissections with early-onset osteoarthritis. Nat. Genet. 43, 121–126 (2011).
Yu, Q. & Stamenkovic, I. Cell surface-localized matrix metalloproteinase-9 proteolytically activates TGF-β and promotes tumor invasion and angiogenesis. Genes Dev. 14, 163–176 (2000).
Habashi, J.P. et al. Angiotensin II type 2 receptor signaling attenuates aortic aneurysm in mice through ERK antagonism. Science 332, 361–365 (2011).
Brooke, B.S. et al. Angiotensin II blockade and aortic-root dilation in Marfan's syndrome. N. Engl. J. Med. 358, 2787–2795 (2008).
Milleron, O. et al. Marfan Sartan: a randomized, double-blind, placebo-controlled trial. Eur. Heart J. 36, 2160–2166 (2015).
Gibbons, G.H., Pratt, R.E. & Dzau, V.J. Vascular smooth muscle cell hypertrophy vs. hyperplasia. Autocrine transforming growth factor-β1 expression determines growth response to angiotensin II. J. Clin. Invest. 90, 456–461 (1992).
Zhou, Y., Poczatek, M.H., Berecek, K.H. & Murphy-Ullrich, J.E. Thrombospondin 1 mediates angiotensin II induction of TGF-β activation by cardiac and renal cells under both high and low glucose conditions. Biochem. Biophys. Res. Commun. 339, 633–641 (2006).
Touyz, R.M. & Schiffrin, E.L. Signal transduction mechanisms mediating the physiological and pathophysiological actions of angiotensin II in vascular smooth muscle cells. Pharmacol. Rev. 52, 639–672 (2000).
Wang, Y. et al. TGF-β activity protects against inflammatory aortic aneurysm progression and complications in angiotensin II-infused mice. J. Clin. Invest. 120, 422–432 (2010).
Carta, L. et al. p38 MAPK is an early determinant of promiscuous Smad2/3 signaling in the aortas of fibrillin-1 (Fbn1)-null mice. J. Biol. Chem. 284, 5630–5636 (2009).
Wassmann, S. et al. Induction of p53 by GKLF is essential for inhibition of proliferation of vascular smooth muscle cells. J. Mol. Cell. Cardiol. 43, 301–307 (2007).
Hsieh, J.K. et al. p53, p21(WAF1/CIP1), and MDM2 involvement in the proliferation and apoptosis in an in vitro model of conditionally immortalized human vascular smooth muscle cells. Arterioscler. Thromb. Vasc. Biol. 20, 973–981 (2000).
Clark, P.R. et al. MEK5 is activated by shear stress, activates ERK5 and induces KLF4 to modulate TNF responses in human dermal microvascular endothelial cells. Microcirculation 18, 102–117 (2011).
Wang, X. & Tournier, C. Regulation of cellular functions by the ERK5 signalling pathway. Cell. Signal. 18, 753–760 (2006).
Humphrey, J.D., Dufresne, E.R. & Schwartz, M.A. Mechanotransduction and extracellular matrix homeostasis. Nat. Rev. Mol. Cell Biol. 15, 802–812 (2014).
Humphrey, J.D., Milewicz, D.M., Tellides, G. & Schwartz, M.A. Cell biology. Dysfunctional mechanosensing in aneurysms. Science 344, 477–479 (2014).
Jovanović, J., Iqbal, S., Jensen, S., Mardon, H. & Handford, P. Fibrillin-integrin interactions in health and disease. Biochem. Soc. Trans. 36, 257–262 (2008).
Wernig, F., Mayr, M. & Xu, Q. Mechanical stretch-induced apoptosis in smooth muscle cells is mediated by β1-integrin signaling pathways. Hypertension 41, 903–911 (2003).
Desmet, F.-O. et al. Human Splicing Finder: an online bioinformatics tool to predict splicing signals. Nucleic Acids Res. 37, e67 (2009).
Brons, I.G.M. et al. Derivation of pluripotent epiblast stem cells from mammalian embryos. Nature 448, 191–195 (2007).
Touboul, T. et al. Generation of functional hepatocytes from human embryonic stem cells under chemically defined conditions that recapitulate liver development. Hepatology 51, 1754–1765 (2010).
Acknowledgements
The authors thank L. Vallier, the hiPSC core facility at the Anne McLaren Laboratory and I. Geti for help in generating the MFS hiPSC lines. We thank N. Figg for sectioning and staining of the teratomas, J. Sterling for help with skin biopsies, J. Skepper at the Cambridge Advance Imaging Centre at the University of Cambridge for the transmission electron microscopy images and C. Verstreken at the Cambridge Stem Cell Institute for providing the static stretching membranes. We also thank Z. Mallat for useful comments on the manuscript. This work was supported by Evelyn Trust, the NIHR Cambridge Biomedical Research Centre and the British Heart Foundation (FS/13/29/30024 (S.S.), RM/l3/3/30159 (S.S. and M.M.) and FS/11/77/29327 (W.B.)).
Author information
Authors and Affiliations
Contributions
A.G., conception, design, acquisition, analysis and interpretation of iPSC-SMC data and to the drafting of the article; F.S., help with conception and design and the analysis of the CRISPR–Cas9 iPSC clones and NC protocol; W.G.B., help with to the neural crest protocol for deriving NC-SMCs; M.M., qPCR analysis of fibroblasts and iPSC-derived SMC lines and the stretch studies; L.L., teratoma assay; P.S., providing human aortic tissue; S.S., conceptual design of the experiments, help with obtaining funding and supervision of all studies. All authors contributed to revision of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Generation and characterization of hiPSCs from MFG880S fibroblasts.
a) DNA sequencing analysis of MFG880S iPSCs showing 2638G>A mutation in FBN1 in exon 21. b) Immunofluorescent staining of representative MFG880S hiPSC clone for pluripotent markers: OCT3/4, SOX2, SSEA4 and TRA-1-60. Nuclear counterstaining performed with DAPI (Insets). c) 46 X,Y normal karyotype of MFC1242Y hiPSC. d) RT-qPCR for the expression of exogenous and endogenous NANOG, v-Myc, OCT3/4, and SOX2 genes. e) RT-qPCR analysis showing expression of specific markers for each of the three germ layers (SOX17, endoderm; BRACHYURY (T), mesoderm; PAX6, ectoderm) in WT, MFC1242Y and MFG880S hiPSCs. f) Differentiation of WT and MFC1242Y into the three germ layers, stained for specific markers: SOX17, endoderm; BRACHYURY, mesoderm; SOX1, ectoderm. g) MFS-hiPSC injected under the skin of DTR/BL6 immunodeficient mice form teratomas containing cells from three germ layers (endoderm, mesoderm and ectoderm; Scale bars, 100μm). The results are presented as means ± SD of three independent experiments. The relative mRNA level in each sample was normalized to its GAPDH and PBGD content.
Supplementary Figure 2 Differentiation of MFC1242Y and MFG880S hiPSCs into three origin-specific SMC lineages.
a) RNA was extracted from WT, MFC1242Y and MFG880S at hiPSC stage, at intermediate population stage (LM, PM, NC), at early SMC differentiation stage (PTD6), at end of the differentiation protocol (PTD12) and at mature stage (S30). WT and MF SMCs show expression of intermediate markers (NKX2.5, lateral mesoderm; TCF15, paraxial mesoderm; p75, neural crest) and expression of SMC markers (CNN1 and MYH11) during differentiation and at mature stages. The results are presented as means ± SD of three independent experiments. b) Immunostaining analysis shows the three intermediate stages (LM, NKX2.5; PM, MEOX1; NC, p75) for WT, MFC1242Y and MFG880S. After 12 days treatment with PT (SMC PTD12), WT, MFC1242Y and MFG880S are stained for SMC markers, including CNN1 and ACTA2 (scale bar=50μm). The results are presented as means ± SD of three independent experiments.
Supplementary Figure 4 MFG880S NC-SMCs show reduced fibrillin-1 accumulation, decreased proliferation and higher caspase activity.
a) Immunostaining analysis of fibrillin-1 in mature MFG880S NC-SMCs (S30) compared to WT (scale bar=50μm). b) Quantification of fibrillin-1 staining relative to cell numbers in WT and MFG880S NC-SMCs. c) RT-qPCR analysis showing expression of FBN1 in WT, MFC1242Y and MFG880S SMC lineages. d) Cropped blot of fibrillin-1 protein in two WT, MFC1242Y and MFG880S NC-SMCs. e) Measurement of TGF-β1 levels in the supernatant of both MFG880S and WT NC-SMCs. Concentration of TGF-β1 is expressed relative to the total protein concentration. f) Total TGF-β1 mRNA levels detected by RT-qPCR in WT and MF SMC lineages. g) Measurement of luciferase activity in the lysates of MLECs (Mink Lung Endothelial Cells) stably transfected with human PAI-1 luciferase reporter, previously incubated with WT, MFC1242Y and MFG880S NC-SMC conditioned media cells. Luciferase activity was expressed relative to protein concentrations. The relative mRNA level in each sample was normalized to its GAPDH and PBGD content. The results are presented as means ± SD of three independent experiments. The asterisks indicate statistically significant differences; * p< 0.05; ** p< 0.01.
Supplementary Figure 5 MFG880S NC-SMCs show functional abnormalities similar to MFC1242Y.
a) Immunostaining for CNN1 of WT and MFG880S NC-SMCs at mature stage (S30). b) Proliferation of WT and MFG880S at NC intermediate, SMC PTD12 and S30 stage was measured by MTT assay. c) A FAM poly-caspase assay was used to detect the percentage of caspase activity and cell death in MFG880S and WT NC-SMCs at S30 stage and quantification of FAM poly-caspase assays shown in Figure 2e. d) Single cell fluorescence tracing of WT and MFG880S NC-SMCs before and after carbachol stimulation (4s), relative to basal level and total Fluo-4AM loading. The results are presented as means ± SD of three independent experiments.
Supplementary Figure 6 Increased levels of phosphorylated TGF-β pathway components and MMPs in WT, MFC1242Y and MFG880S SMCs at PTD12.
a) Cropped blots of phosphorylated SMAD2 (canonical), ERK1/2 and p38 (non-canonical) in WT, MFC1242Y and MFG880S fibroblasts and NC-SMCs at D12PT. b) Expression profile of MMP1, MMP9 and MMP10 in WT and MFC1242Y fibroblast lines. c-d) A range of MMPs and TIMPs, including MMP1, MMP9, MMP10 and TIMP1, TIMP2, TIMP3 in MFC1242Y, MFG880S and WT PTD12 NC-SMCs. e) FITC-gel degradation assay comparing WT and MFG880S NC-SMCs after 24h of culture, stained with CNN1 (red) and quantification of the area of matrix degradation relative to cell numbers. The relative mRNA level in each sample was normalized to its GAPDH and PBGD content. The results are presented as means ± SD of three independent experiments. The asterisk indicates statistically significant difference (*** p< 0.001).
Supplementary Figure 7 Effectiveness of TGF-β inhibition and of dox in preventing ECM degradation and increasing fibrillin-1 accumulation.
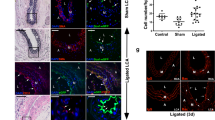
a) Schematic of the timing of NC-SMC treatment with different inhibitors and siRNA transfection. b) MMP1, MMP9 and MMP10 mRNA expression profile in WT and MFC1242Y NC-SMCs after treatment with TGF-β neutralizing antibody and Losartan at PTD12. The relative mRNA level in each sample was normalized to its GAPDH and PBGD content. c) FITC-gelatin assay shows degradation in WT and MFC1242Y NC-SMC control and upon treatment with Doxycycline (DOX) and Losartan (LOS). Cells were fixed and stained for CNN1 (red). d) Quantification of FITC-gelatin areas of degradation relative to nuclei numbers in MF and WT NC-SMC control (CTL), treated with Doxycycline (DOX) and Losartan. e-f) Immunostaining and quantification of fibrillin-1 levels in the matrix in control (CTL) and sample treated with Doxycycline (DOX) for 6 days. g) Measurement of TGF-β1 levels by ELISA in the supernatant of WT and MFC1242Y fibroblasts, NC-SMC control (CTL) and after treatment with Doxycycline (DOX). Concentration of TGF-β1 is expressed relative to the total protein concentration. The results are presented as means ± SD of three independent experiments. The asterisks indicate statistically significant differences; * p< 0.05; **p<0.01; *** p< 0.01.
Supplementary Figure 8 WT and MFC1242Y SMC survival and death are not significantly altered upon losartan treatment.
a) Poly-caspase assay shows caspase activity and cell death detected by propidium iodide (PI) by flow cytometry in both WT (blue) and MFC1242Y NC-SMCs (red) control and after treatment with Losartan (represented in green in WT and purple in MFC1242Y) at S30. The results are presented as means ± SD of two independent experiments.
Supplementary Figure 9 Quantification of P-SMAD2, P-ERK1/2 and P-p38 upon treatment with specific inhibitors.
a) Cropped blots of P-SMAD2, P-ERK1/2 and P-p38 in control cells (CTL), and samples treated with SB431542, SB203580, PD98059 and Losartan (LOS). b) Quantification of the phosphorylated SMAD2, ERK1/2 and p38 protein levels relative to β-actin in CTL and samples treated with SB431542 (ALK5 inhibitor), SB203580 (p38 inhibitor) and PD98059 (ERK1/2 inhibitor). The results are representative of three independent experiments (means ± SD). The asterisks indicate statistically significant differences; * p< 0.05; **p<0.01; *** p< 0.01.
Supplementary Figure 10 Effects of inhibiting TGF-β-specific pathways on fibrillin-1 accumulation and cell death and viability in MFG880S NC-SMCs.
a) Immunostaining of fibrillin-1 in S30 WT and MFG880S NC-SMCs after treatment with a range of inhibitors: CTL= control; SB431542 (ALK5 inhibitor); SB203580 (p38 inhibitor); PD98059 (ERK1/2 inhibitor) and Losartan (AGTR1 inhibitor). b) Quantification of fibrillin-1 staining relative to cell number (nuclei). c) Flow cytometric analysis of AnnexinV in WT and MFC1242Y fibroblast lines. d) AnnexinV staining to determine apoptosis levels of WT and MFG880S NC-SMCs following treatment with SB203580, Losartan, PD98059 (ERK1/2 inhibition) and by transfection with KLF4 siRNA. The result is representative of three independent experiments (means ± SD). The asterisks indicate statistically significant differences (**p<0.01).
Supplementary Figure 11 KLF4 inhibits MFS NC-SMC proliferation and is regulated by ERK5.
a) KLF4 expression prolife in WT, MFC1242Y and MFG880S NC-SMCs detected by RT-qPCR. b) BrdU staining was used to measure the proliferation rate of WT, MFC1242Y and MFG880S NC-SMCs 3 days after transfection with KLF4 siRNA (siRKLF4) compared to the mock siRNA (siScr). c) Quantification of BrdU staining represented as percentage of BrdU-positive cells in WT and MF NC-SMCs transfected with siScr or SiRKLF4 relative to cell number (nuclei). d) KLF4 mRNA profile in WT and MF fibroblasts and in NC-SMC CTL and upon treatment with a series of inhibitors (BIX02189, SB431542, SB203580, PD98059 and Losartan). e) mRNA expression analysis of CDKN1A (p21), CCND1 (CYCLIN D1) and TP53 (p53) in WT and MFC1242Y NC-SMC control and upon treatment with BIX02189 (MK5/ERK5 inhibitor) and anti-TGF-β neutralizing antibody (α-TGF-β Ab). The results are presented as means ± SD of two independent experiments. The asterisk indicates statistically significant difference * p< 0.05; ** p< 0.01.
Supplementary Figure 12 MF NC-SMC apoptosis is affected negatively by treatment with U0126 (ERK1/2 inhibitor) and positively by plasmin inhibition.
a) Flow cytometric analysis shows annexinV-positive apoptotic population in both WT and MFC1242Y NC-SMC control and samples treated with U0126 (ERK1/2 inhibition). b) Apoptosis levels measured by flow cytometric analysis adding Propidium Iodide (PI) to CTL cells and SMC treated with α2-antiplasmin neutralizing antibody for 24h to block plasmin activity. The results are representative of two independent experiments (means ± SD).
Supplementary Figure 13 Expression profile of β1 integrin in different SMC lineages.
a) RT-qPCR analysis of β1 integrin mRNA levels in WT and MFC1242Y LM-, PM- and NS-SMCs. b) Flow cytometric analysis of β1 integrin protein (β1-APC) expression profile in WT and MFC1242Y SMC lineages. The results are representative of three independent experiments (means ± SD). The asterisk indicates statistically significant difference * p< 0.05; ** p< 0.01.
Supplementary Figure 14 MFC1242Y CRISPR–Cas9 gene editing strategy.
a-b) Strategy for the correction of the FBN1 mutation CYS1242TYR using CRISPR/Cas9 technology. a1) FBN1 exon 30 wild-type genomic location (MF CYS1242TYR mutation is shown as a red triangle). a2-3) P1 and P2 (primers) were used to PCR out 1,063 bp upstream and 970 bp downstream of exon 30 from wild type genomic DNA. Two restriction sites were created into the intron sequence upstream of exon 30 (KpnI and BclI) and the construct piggyBac transposon with the selectable marker puroR was inserted to generate the final donor plasmid. ClaI restriction site in exon 30 was removed by direct-mutagenesis to generate a silent point mutation in the donor plasmid to facilitate posterior screening. b1) FBN1 exon 30 following Cas9 cleavage. b2) Final donor plasmid with intronic homology arms surrounding FBN1 exon 30 (LHA and RHA) for specific homology direct repair (HDR) with genomic DNA. b3) Insertion of the donor plasmid following homologous recombination after cas9 genomic DNA cutting. c) Partial sequences of FBN1 exon 30. MF CRISPR/cas9 mutant allele (CRISPR MF mutant, top panel) and MF CRISPR/cas9 corrected allele (CRISPR MF corrected bottom panel). ClaI site point-mutation shows that only one allele was edited with CRISPR/cas9. d) Characterization of CRISPR MF mutant and corrected lines by immunostaining for hiPSC pluripotency (OCT3/4; a,d), NC differentiation (p75; b-e) and NC-SMC differentiation (CNN1; c-f). Scale bar=50μm.
Supplementary Figure 15 CRISPR–Cas9-mediated correction reverts MFS phenotype.
a) Proliferation rate detected by BrdU labeling in CRISPR MF corrected compared to MFC1242Y and CRISPR MF mutant NC-SMCs. b) Quantification of BrdU in MFC1242Y, CRISPR MF mutant and MF corrected NC-SMCs as percentage of BrdU positive cells relative to cell number (DAPI). c) Levels of TGF-β1 detected by ELISA in the supernatant of CRISPR MF correct, CRISPR MF mutant and MFC1242Y NC-SMCs. d) Expression analysis of MMP10 by RT-qPCR in CRISPR MF correct, CRISPR MF mutant and MFC1242Y NC-SMCs. e) Degradation activity was measured by FITC-GEL assay in CRISPR MF correct and CRISPR MF mutant NC-SMCs, stained positive for the SMC marker, CNN1. f) Quantification of FITC-GEL degradation relative to cells number (nuclei) in CRISPR MF mutant and correct SMC. The results are presented as means ± SD of three independent experiments. The asterisk indicates statistically significant difference * p< 0.05; **p<0.01; *** p< 0.001.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–15, Supplementary Tables 1–5 and Supplementary Note (PDF 3705 kb)
Rights and permissions
About this article
Cite this article
Granata, A., Serrano, F., Bernard, W. et al. An iPSC-derived vascular model of Marfan syndrome identifies key mediators of smooth muscle cell death. Nat Genet 49, 97–109 (2017). https://doi.org/10.1038/ng.3723
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.3723
This article is cited by
-
In vivo phenotypic vascular dysfunction extends beyond the aorta in a mouse model for fibrillin-1 (Fbn1) mutation
Scientific Reports (2024)
-
Multi-omics in thoracic aortic aneurysm: the complex road to the simplification
Cell & Bioscience (2023)
-
Functional genomics in stroke: current and future applications of iPSCs and gene editing to dissect the function of risk variants
BMC Cardiovascular Disorders (2023)
-
Development of vascular disease models to explore disease causation and pathomechanisms of rare vascular diseases
Seminars in Immunopathology (2022)
-
Novel LTBP3 mutations associated with thoracic aortic aneurysms and dissections
Orphanet Journal of Rare Diseases (2021)