Abstract
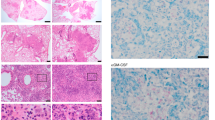
Nitric oxide contributes to protection from tuberculosis. It is generally assumed that this protection is due to direct inhibition of Mycobacterium tuberculosis growth, which prevents subsequent pathological inflammation. In contrast, we report that nitric oxide primarily protects mice by repressing an interleukin-1- and 12/15-lipoxygenase-dependent neutrophil recruitment cascade that promotes bacterial replication. Using M. tuberculosis mutants as indicators of the pathogen's environment, we inferred that granulocytic inflammation generates a nutrient-replete niche that supports M. tuberculosis growth. Parallel clinical studies indicate that a similar inflammatory pathway promotes tuberculosis in patients. The human 12/15-lipoxygenase orthologue, ALOX12, is expressed in cavitary tuberculosis lesions; the abundance of its products correlates with the number of airway neutrophils and bacterial burden and a genetic polymorphism that increases ALOX12 expression is associated with tuberculosis risk. These data suggest that M. tuberculosis exploits neutrophilic inflammation to preferentially replicate at sites of tissue damage that promote contagion.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Canetti, G. The tubercle bacillus in the pulmonary lesion of man. Am. J. Med. Sci. 231, 480 (1956).
Mishra, B. B. et al. Nitric oxide controls the immunopathology of tuberculosis by inhibiting NLRP3 inflammasome-dependent processing of IL-1β. Nat. Immunol. 14, 52–60 (2013).
Niazi, M. K. K. et al. Lung necrosis and neutrophils reflect common pathways of susceptibility to Mycobacterium tuberculosis in genetically diverse, immune-competent mice. Dis. Model. Mech. 8, 1141–1153 (2015).
Mattila, J. T., Maiello, P., Sun, T., Via, L. E. & Flynn, J. L. Granzyme B-expressing neutrophils correlate with bacterial load in granulomas from Mycobacterium tuberculosis-infected cynomolgus macaques. Cell. Microbiol. 17, 1085–1097 (2015).
Berry, M. P. R. et al. An interferon-inducible neutrophil-driven blood transcriptional signature in human tuberculosis. Nature 466, 973–977 (2010).
Scanga, C. A. et al. The inducible nitric oxide synthase locus confers protection against aerogenic challenge of both clinical and laboratory strains of Mycobacterium tuberculosis in mice. Infect. Immun. 69, 7711–7717 (2001).
Flynn, J. L., Scanga, C. A., Tanaka, K. E. & Chan, J. Effects of aminoguanidine on latent murine tuberculosis. J. Immunol. 160, 1796–1803 (1998).
Tsiganov, E. N. et al. Gr-1dimCD11b+ immature myeloid-derived suppressor cells but not neutrophils are markers of lethal tuberculosis infection in mice. J. Immunol. 192, 4718–4727 (2014).
Knaul, J. K. et al. Lung-residing myeloid-derived suppressors display dual functionality in murine pulmonary tuberculosis. Am. J. Respir. Crit. Care Med. 190, 1053–1066 (2014).
Obregón-Henao, A., Henao-Tamayo, M., Orme, I. M. & Ordway, D. J. Gr1(int)CD11b+ myeloid-derived suppressor cells in Mycobacterium tuberculosis infection. PLoS ONE 8, e80669 (2013).
MacMicking, J. D. Interferon-inducible effector mechanisms in cell-autonomous immunity. Nat. Rev. Immunol. 12, 367–382 (2012).
Jayaraman, P. et al. IL-1β promotes antimicrobial immunity in macrophages by regulating TNFR signaling and caspase-3 activation. J. Immunol. 190, 4196–4204 (2013).
Fremond, C. M. et al. IL-1 receptor-mediated signal is an essential component of MyD88-dependent innate response to Mycobacterium tuberculosis infection. J. Immunol. 179, 1178–1189 (2007).
Zhang, G. et al. Allele-specific induction of IL-1β expression by C/EBPβ and PU.1 contributes to increased tuberculosis susceptibility. PLoS Pathogens 10, e1004426 (2014).
Nouailles, G. et al. CXCL5-secreting pulmonary epithelial cells drive destructive neutrophilic inflammation in tuberculosis. J. Clin. Invest. 124, 1268–1282 (2014).
Irwin, S. M. et al. Presence of multiple lesion types with vastly different microenvironments in C3HeB/FeJ mice following aerosol infection with Mycobacterium tuberculosis. Dis. Model. Mech. 8, 591–602 (2015).
Padgett, E. L. & Pruett, S. B. Rat, mouse and human neutrophils stimulated by a variety of activating agents produce much less nitrite than rodent macrophages. Immunology 84, 135–141 (1995).
Denis, M. Human neutrophils, activated with cytokines or not, do not kill virulent Mycobacterium tuberculosis. J. Infect. Dis. 163, 919–920 (1991).
Long, J. E. et al. Identifying essential genes in Mycobacterium tuberculosis by global phenotypic profiling. Methods Mol. Biol. 1279, 79–95 (2015).
Padilla-Benavides, T., Long, J. E., Raimunda, D., Sassetti, C. M. & Argüello, J. M. A novel P(1B)-type Mn2+-transporting ATPase is required for secreted protein metallation in mycobacteria. J. Biol. Chem. 288, 11334–11347 (2013).
Nambi, S. et al. The oxidative stress network of Mycobacterium tuberculosis reveals coordination between radical detoxification systems. Cell Host Microbe 17, 829–837 (2015).
Darwin, K. H., Ehrt, S., Gutierrez-Ramos, J.-C., Weich, N. & Nathan, C. F. The proteasome of Mycobacterium tuberculosis is required for resistance to nitric oxide. Science 302, 1963–1966 (2003).
Cambier, C. J. et al. Mycobacteria manipulate macrophage recruitment through coordinated use of membrane lipids. Nature 505, 218–222 (2014).
Quadri, L. E., Sello, J., Keating, T. A., Weinreb, P. H. & Walsh, C. T. Identification of a Mycobacterium tuberculosis gene cluster encoding the biosynthetic enzymes for assembly of the virulence-conferring siderophore mycobactin. Chem. Biol. 5, 631–645 (1998).
Forrellad, M. A. et al. Role of the Mce1 transporter in the lipid homeostasis of Mycobacterium tuberculosis. Tuberculosis (Edinb.) 94, 170–177 (2014).
Kendall, S. L. et al. A highly conserved transcriptional repressor controls a large regulon involved in lipid degradation in Mycobacterium smegmatis and Mycobacterium tuberculosis. Mol. Microbiol. 65, 684–699 (2007).
Marrero, J., Rhee, K. Y., Schnappinger, D., Pethe, K. & Ehrt, S. Gluconeogenic carbon flow of tricarboxylic acid cycle intermediates is critical for Mycobacterium tuberculosis to establish and maintain infection. Proc. Natl Acad. Sci. USA 107, 9819–9824 (2010).
Dennis, E. A. & Norris, P. C. Eicosanoid storm in infection and inflammation. Nat. Rev. Immunol. 15, 511–523 (2015).
Kashino, S. S., Ovendale, P., Izzo, A. & Campos-Neto, A. Unique model of dormant infection for tuberculosis vaccine development. Clin. Vaccine Immunol. 13, 1014–1021 (2006).
Lämmermann, T. et al. Neutrophil swarms require LTB4 and integrins at sites of cell death in vivo. Nature 498, 371–375 (2013).
Van Leyen, K. et al. Baicalein and 12/15-lipoxygenase in the ischemic brain. Stroke 37, 3014–3018 (2006).
Reynaud, D. & Pace-Asciak, C. R. 12-HETE and 12-HPETE potently stimulate intracellular release of calcium in intact human neutrophils. Prostaglandins Leukot. Essent. Fatty Acids 56, 9–12 (1997).
Mrsny, R. J. et al. Identification of hepoxilin A3 in inflammatory events: a required role in neutrophil migration across intestinal epithelia. Proc. Natl Acad. Sci. USA 101, 7421–7426 (2004).
Tobin, D. M. et al. The lta4h locus modulates susceptibility to mycobacterial infection in zebrafish and humans. Cell 140, 717–730 (2010).
Marakalala, M. J. et al. Inflammatory signaling in human tuberculosis granulomas is spatially organized. Nat. Med. 22, 531–538 (2016).
McDonald, B. et al. Intravascular danger signals guide neutrophils to sites of sterile inflammation. Science 330, 362–366 (2010).
Hurley, B. P., Pirzai, W., Mumy, K. L., Gronert, K. & McCormick, B. A. Selective eicosanoid-generating capacity of cytoplasmic phospholipase A2 in Pseudomonas aeruginosa-infected epithelial cells. Am. J. Physiol. Lung Cell Mol. Physiol. 300, L286–L294 (2011).
Tamang, D. L. et al. Hepoxilin A(3) facilitates neutrophilic breach of lipoxygenase-expressing airway epithelial barriers. J. Immunol. 189, 4960–4969 (2012).
Bhowmick, R. et al. Systemic disease during Streptococcus pneumoniae acute lung infection requires 12-lipoxygenase-dependent inflammation. J. Immunol. 191, 5115–5123 (2013).
Mayer-Barber, K. D. et al. Host-directed therapy of tuberculosis based on interleukin-1 and type I interferon crosstalk. Nature 511, 99–103 (2014).
Laskay, T., van Zandbergen, G. & Solbach, W. Neutrophil granulocytes—Trojan horses for Leishmania major and other intracellular microbes? Trends Microbiol. 11, 210–214 (2003).
Herron, M. J. et al. Intracellular parasitism by the human granulocytic ehrlichiosis bacterium through the P-selectin ligand, PSGL-1. Science 288, 1653–1656 (2000).
Winter, S. E., Lopez, C. A. & Bäumler, A. J. The dynamics of gut-associated microbial communities during inflammation. EMBO Rep. 14, 319–327 (2013).
Kim, M.-J. et al. Caseation of human tuberculosis granulomas correlates with elevated host lipid metabolism. EMBO Mol. Med. 2, 258–274 (2010).
Owens, C. P. et al. The Mycobacterium tuberculosis secreted protein Rv0203 transfers heme to membrane proteins MmpL3 and MmpL11. J. Biol. Chem. 288, 21714–21728 (2013).
Nandi, B. & Behar, S. M. Regulation of neutrophils by interferon-γ limits lung inflammation during tuberculosis infection. J. Exp. Med. 208, 2251–2262 (2011).
Palace, S. G., Proulx, M. K., Lu, S., Baker, R. E. & Goguen, J. D. Genome-wide mutant fitness profiling identifies nutritional requirements for optimal growth of Yersinia pestis in deep tissue. mBio 5, e01385–14 (2014).
Zhang, G. et al. An SNP selection strategy identified IL-22 associating with susceptibility to tuberculosis in Chinese. Sci. Rep. 1, 20 (2011).
Chen, X. et al. Diagnosis of active tuberculosis in China using an in-house gamma interferon enzyme-linked immunospot assay. Clin. Vaccine Immunol. 16, 879–884 (2009).
Guan, Y. Q., Cai, Y. Y., Zhang, X., Lee, Y. T. & Opas, M. Adaptive correction technique for 3D reconstruction of fluorescence microscopy images. Microsc. Res. Tech. 71, 146–157 (2008).
Acknowledgements
This work was supported by grants from the Natural Science Foundation of China (81525016, 81501714 and 81500004 to X.C.), the National Institutes of Health (NIH; AI064282 and AI107774 to C.M.S., AI120556 to R.R.L., AI003749 to S.G.P. and MH096625 to E.E.) and the Arnold and Mabel Beckman Foundation (to A.J.O.). The authors thank C. Moss for providing technical help, S.M. Behar for critical review of the manuscript and the UMMS Department of Animal Medicine for Animal Care.
Author information
Authors and Affiliations
Contributions
B.B.M. and C.M.S. conceived and designed the study. B.B.M., R.R.L. and A.J.O. performed mouse experiments. G.Z., W.W. and X.C. designed and performed the SNP study in Chinese cohorts. E.E. and V.D. designed and performed the IHC study of the lung biopsies from TB patients, and analysed data. S.G.P., S.N., C.M.S., M.G.B., R.N., C.E.B. and J.P.Y. provided technical help during various experiments. M.L.D. and S.A.S. performed LC–MS analysis. B.B.M., R.R.L. and C.M.S. analysed the data. B.B.M. and C.M.S. wrote the manuscript and C.M.S. supervised the overall study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Information
Supplementary Figures 1–9, Supplementary Tables 4 and 5, Supplementary References. (PDF 12347 kb)
Supplementary Table 1
Genome-wide fitness profiling of Mtb mutants in C57BL/6, C3HeB and NOS2-deficient mice. (XLSX 1239 kb)
Supplementary Table 2
Mutants significantly altered in C3HeB and Nos2 KO mice compared to C57BL/6 mice. (XLSX 47 kb)
Supplementary Table 3
Polymorphisms used for genotyping human cohorts. (XLSX 59 kb)
Rights and permissions
About this article
Cite this article
Mishra, B., Lovewell, R., Olive, A. et al. Nitric oxide prevents a pathogen-permissive granulocytic inflammation during tuberculosis. Nat Microbiol 2, 17072 (2017). https://doi.org/10.1038/nmicrobiol.2017.72
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/nmicrobiol.2017.72
This article is cited by
-
An innate granuloma eradicates an environmental pathogen using Gsdmd and Nos2
Nature Communications (2023)
-
BCGΔBCG1419c increased memory CD8+ T cell-associated immunogenicity and mitigated pulmonary inflammation compared with BCG in a model of chronic tuberculosis
Scientific Reports (2022)
-
Early alveolar macrophage response and IL-1R-dependent T cell priming determine transmissibility of Mycobacterium tuberculosis strains
Nature Communications (2022)
-
Anti-tuberculosis treatment strategies and drug development: challenges and priorities
Nature Reviews Microbiology (2022)
-
Ifnar gene variants influence gut microbial production of palmitoleic acid and host immune responses to tuberculosis
Nature Metabolism (2022)