Abstract
Deep brain stimulation (DBS) of subcallosal cingulate white matter (SCC) may be an effective approach for treatment-resistant depression (TRD) that otherwise fails to respond to more conventional therapies, but DBS is invasive, costly, and has potential for adverse effects. Therefore, it is important to identify potential biomarkers for predicting antidepressant response before intervention. Resting-state EEG was recorded from 12 TRD patients at pre-treatment baseline, after 4 weeks SCC DBS, and after 24 weeks SCC DBS. Lower frontal theta cordance (FTC) at baseline (and higher FTC after 4 weeks) predicted lower depression severity scores after 24 weeks. Greater FTC increases (baseline–4 weeks) predicted greater decreases in depression severity scores subsequently (4–24 weeks) and over the course of the study (baseline–24 weeks). Predictive relationships were topographically specific to theta cordance for frontal electrodes. Thus, results from this pilot study suggest that baseline FTC and changes early in treatment each have utility as biomarkers for predicting 6-month clinical response to SCC DBS for TRD.
Similar content being viewed by others
INTRODUCTION
Deep brain stimulation (DBS) provides an adjustable and reversible way to modulate activity in targeted brain regions hypothesized to be dysfunctional in a specific psychological/behavioral disorder (Kringelbach et al, 2007; Lozano et al, 2008). Although the underlying mechanisms remain unclear (Kringelbach et al, 2007), DBS has shown clinical utility for Parkinson's disease, dystonia, and essential tremor; with other studies investigating its efficacy for treatment of epilepsy, Tourette's syndrome, obsessive compulsive disorder among other neurological and psychiatric conditions. DBS is currently being tested for treatment-resistant depression (TRD), with preliminary studies showing antidepressant efficacy for chronic stimulation of the subcallosal cingulate white matter (SCC), ventral capsule, and nucleus accumbens (Bewernick et al, 2010; Holtzheimer et al, 2012; Kennedy et al, 2011; Lozano et al, 2008; Malone et al, 2009; Mayberg et al, 2005). The SCC, the most ventral portion of the cingulate gyrus, is postulated to be a critical node in a distributed limbic–cortical network responsible for regulating emotional states and mediating depressive symptoms (Mayberg, 1997, 2009). Anatomical and functional abnormalities in this putative network have been mapped using various neuroimaging techniques with consistent involvement of frontal cortex across studies (Davidson et al, 2002; Hasler and Northoff, 2011; Mayberg, 2009; Price and Drevets, 2010, 2012). Based on these theoretical assumptions and observations, SCC has been targeted with DBS for TRD.
Extending open label studies (Kennedy et al, 2011; Lozano et al, 2008; Mayberg et al, 2005; Holtzheimer et al, 2012) reported a 1-month single-blind sham-lead in study of 10 unipolar and 7 bipolar TRD patients undergoing chronic SCC DBS. Replicating past findings, significant decreases in depression severity scores were associated with DBS. However, because of invasiveness, cost, and potential for adverse effects, it is important to identify biomarkers that can predict antidepressant response before intervention. Therefore, this study examined potential biomarkers of antidepressant response to SCC DBS in resting-state quantitative EEG (QEEG) for 12 patients in the study reported by Holtzheimer et al (2012).
The present investigation of potential QEEG biomarkers of antidepressant response to SCC DBS focused on rhythms in theta frequency (4–8 Hz). EEG theta frequencies are generated by various sources in the human brain including medial prefrontal cortex (PFC), anterior cingulate cortex (ACC), hippocampus, amygdala, thalamus, as well as multiple striato-cortical circuits (Asada et al, 1999; Knyazev, 2007; Sauseng and Klimesch, 2008). These structures (and theta oscillations) are functionally associated variously with attention, memory, and learning; as well as emotional processing and self-oriented cognition (Knyazev, 2007; Sauseng et al, 2010; Sauseng and Klimesch, 2008)—functions characteristically impacted by depressive disorders. Furthermore, likely theta generators are much overlapping with the distributed limbic–cortical network hypothesized to be dysfunctional in major depressive disorder—and which is targeted by SCC DBS for TRD (Mayberg, 2009). For these reasons, QEEG theta measures were selected as likely to show predictive associations with antidepressant response to treatment by SCC DBS.
Indeed, many prior investigations have focused on midline frontal theta in relation to depressive states and changes in these, in response to antidepressant treatment by medications. Using low-resolution electromagnetic tomography, Korb et al (2008) found that current source density (CSD) across a range of frequencies including theta, localized to ACC and PFC, was found to be higher for patients with major depressive disorder compared with healthy controls. Additionally, Pizzagalli et al (2001, 2002 ) and Mulert et al (2007) found that higher theta CSD at pre-treatment baseline localized to rostral ACC predicted better clinical response to antidepressant medications, consistent with findings using PET measures of regional glucose metabolism (Pizzagalli et al, 2003).
Another method for quantifying EEG frequency information, which has been applied extensively to predicting clinical response to antidepressant medications, is called cordance (Leuchter et al, 1994). Cordance is a linear combination of normalized absolute power and relative power in a specific frequency band at a specific recording site (additional details are provided in Participants and methods section), originally proposed as a QEEG measure for detecting cortical deafferentation (because of, eg, white matter lesions). Theta cordance is widely interpreted as reflecting local energy consumption in PFC and ACC (Leuchter and Cook, 2010). In previous studies in which patients were treated by antidepressant medications, frontal theta cordance (FTC) decreases from pre-treatment baseline have predicted better clinical response (Bares et al, 2008, 2010, 2012; Cook et al, 2002, 2009; Hunter et al, 2010). Additionally, Bares et al (2012) found higher FTC at baseline for clinical responders compared with non-responders. Based on such prior findings, FTC was selected as likely to show predictive associations with antidepressant response to treatment by SCC DBS.
Present Study
EEG was recorded at three time points from 12 patients with TRD undergoing treatment by SCC DBS: at pre-treatment baseline, after 4 weeks DBS, and after 24 weeks DBS. Theta cordance values at frontal and posterior recording sites were examined to identify potential predictors of antidepressant response. Two main questions were addressed: (1) would FTC at baseline predict antidepressant response, and (2) would early changes in FTC predict antidepressant response? It was expected that FTC at pre-treatment baseline and FTC changes early after treatment onset would both predict antidepressant response to treatment by SCC DBS.
PARTICIPANTS AND METHODS
Participants
Data from 12 patients enrolled in a SCC DBS study for TRD (7 women; mean age=40.42 years, SD=9.78) were included based on eligibility criteria reported previously (Holtzheimer et al, 2012). Briefly, patients were diagnosed with either major depressive disorder (n=9) or bipolar II disorder, depressed (n=3), had a current depressive episode of at least 12 months, had failed at least four adequate antidepressant treatments including electroconvulsive therapy, and had no other major psychiatric or medical comorbidity (additional patient demographic characteristics and history are reported in Table 1). Patients remained on current medications with doses stable for at least 4 weeks before DBS surgery and throughout the 24 weeks of active DBS. Patients were prescribed a variety of medications including in many cases common antidepressant medications and mood stabilizers. The study protocol was approved by the Institutional Review Boards at Georgia Institute of Technology and Emory University. Participants gave written informed consent.
Procedure
DBS. DBS parameters were similar at both time points subsequent to pre-treatment baseline (130 Hz, 90 ms pulse width, 6–8 mA current). Additional details concerning location of anatomical target brain tissue, surgery, electrode implantation, stimulation parameters, and so on, are reported in Holtzheimer et al (2012), as well as in Mayberg et al (2005) and Hamani et al (2009). To avoid gross stimulation artifact, DBS was discontinued just before each EEG recording session (and was re-started at the conclusion). There were no acute changes in behavior or self-report with discontinuation of DBS in any of the patients.
Hamilton depression rating scale (HDRS). The 17-item HDRS (Hamilton, 1960) was used to assess depression severity throughout the study. For the following analyses, HDRS scores closest to the time of EEG recording were examined.
Electrophysiological recording and offline data preparation. To minimize potential drowsiness during resting-state EEG recording, patients were seated at a workstation and were asked to keep their eyes open while maintaining fixation on a cross presented centrally on the computer monitor. Furthermore, a researcher was present in the room during EEG recording to monitor patients for drowsiness. EEG was recorded from each participant at rest for 4 min using a BioSemi Active-Two amplifier system (Amsterdam, The Netherlands). Data were digitized at 1024 Hz. Scalp potentials were recorded from 32 channels: FP1/2, F7/8, F3/4, Fz, C3/4, Cz, P7/8, P3/4, Pz, T7/8, O1/2, Oz, AF3/4, FC1/2, CP1/2, PO3/4, FC5/6, and CP5/6. Two additional electrodes were the common mode sense and driven right leg. Vertical electrooculogram (EOG) was calculated offline as the difference between electrodes positioned above and below the left eye. Horizontal EOG was calculated offline as the difference between electrodes positioned on the outer canthi of the left and right eyes.
Offline, scalp channels were re-referenced to form bipolar channels with their immediate neighbors (eg, F4–F8, F4–AF4, F4–FC6, F4–FC2). Digital filtering was done offline using a band-pass 0.1–50 Hz zero phase shift Butterworth filter (12 dB/oct). Continuous EEG was partitioned into 4-s segments. Segments were baseline corrected by setting the average of the first 50 ms of the epoch to zero. Artifact correction was conducted by rejecting segments from all bipolar and EOG channels containing activity greater than ±200 μV. Next, a fast-Fourier transform (FFT) was performed in the power domain with a Hamming window with 50% overlap. The FFT results were averaged over all the segments to yield average power during the 4-min recording session.
Theta cordance. Dependent measures of theta cordance combined absolute and relative power in the theta frequency band (Cook et al, 2009). First, power in four frequency bands including delta (0.5–3.5 Hz), theta (3.5–7.5 Hz), alpha (7.5–12.5 Hz), and beta (12.5–20 Hz) was averaged for bipolar pairs of neighboring electrodes to obtain absolute power for each frequency, at each electrode, for each individual. Next, relative theta power at each electrode was obtained by dividing absolute theta power by total power summed across the four frequency bands. Then, absolute and relative theta power values at each electrode were normalized by dividing by the maximum values of absolute and relative theta power, respectively, recorded across the set of electrodes for each individual.
Normalized absolute and relative theta power values (‘Anorm’ and ‘Rnorm,’ respectively) were then added together, to obtain theta cordance for each of three frontal electrodes (F3, Fz, and F4), according to the formula provided by Cook et al (2009): Cordance(s,f)=Anorm(s,f)+Rnorm(s,f), where s and f refer to site and frequency, respectively. Finally, the dependent measure of FTC was obtained by averaging theta cordance values obtained for F3, Fz, and F4 electrodes. To evaluate the topographical specificity of results, a dependent measure of posterior theta cordance (PTC) was also obtained by averaging cordance values at P3, Pz, and P4 electrodes (calculated using the method just described for F3, Fz, and F4).
RESULTS
Hamilton Depression Rating Scale
Clinical response was defined as ⩾50% HDRS decrease from pre-treatment baseline. According to this criterion, six patients were classified as clinical responders and six as non-responders after 24 weeks of DBS. Table 2 reports HDRS at three time points. Helmert contrasts showed that for responders, HDRS was different at baseline compared with later time points, F(1,5)=25.66, p=0.004, ηp2=0.84, and different at 4 weeks compared with 24 weeks, F(1,5)=48.60, p=0.001, ηp2=0.91. HDRS for non-responders was different at baseline compared with later time points, F(1,5)=27.33, p=0.003, ηp2=0.84, but not at 4 weeks compared with 24 weeks, F(1,5)=1.42, p=0.287, ηp2=0.22.
Theta Cordance
Table 2 reports FTC and PTC at three time points. A mixed-model repeated-measures ANOVA was performed on the dependent variable theta cordance, with time point (baseline, 4 weeks, 24 weeks) and location (FTC, PTC) as within-subjects variables and clinical response (responder, non-responder) as between-subjects variable. The main effects of time point and clinical response were not statistically significant, F<1. The main effect of location was significant, F(1,10)=42.29, p<0.001, ηp2=0.809, and was not qualified by interactions with time point, F<1, or clinical response, F=1.48, p=0.252, ηp2=0.129. Theta cordance was higher at posterior (M=0.899, SD=0.38) vs frontal recording sites (M=0.594, SD=0.30).
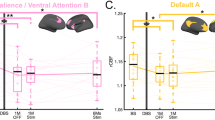
The interaction of time point and clinical response just failed to reach statistical significance, F(2,9)=3.42, p=0.053, ηp2=0.255, ɛ=1. In a sample of only 12 patients, this result might be characterized as a credible trend (Supplementary Figure S1, left panel). Helmert contrasts showed that for responders, theta cordance was significantly different at baseline compared with later time points, F(1,5)=7.29, p=0.043, but was not different at 4 weeks compared with 24 weeks, F<1. For non-responders, theta cordance was not significantly different at baseline compared with later time points, F(1,5)=1.52, p=0.272. The three-way interaction of time point, location, and clinical response was not significant, F(2,9)=1.12, p=0.342, ηp2=0.102, ɛ=1.
Correlations
Table 3 reports correlations among FTC, PTC, and HDRS at three time points (Predictive utility for absolute as well as relative frontal theta power was examined, but no correlations with HDRS were statistically significant, p>0.05.). Notably, FTC at pre-treatment baseline and after 4 weeks each significantly predicted HDRS after 24 weeks, r=0.623, p=0.031 (Supplementary Figure S2, left panel), and r=−0.576 (Supplementary Figure S2, right panel), p=0.050, respectively. To evaluate topographical specificity of results, correlations between FTC at three time points and HDRS at 24 weeks were re-examined in partial correlations controlling for variance shared with PTC at 24 weeks. The partial correlation between FTC at baseline and HDRS at 24 weeks, r=0.563, p=0.071, was reduced compared with the zero-order correlation and no longer significant, as was that between FTC at 4 weeks and HDRS at 24 weeks, r=−0.515, p=0.105. However, the partial correlation between FTC at 24 weeks and HDRS at 24 weeks, r=0.217, p=0.522, was positive (and still nonsignificant), in contrast to the negative zero-order correlation (When the sign of a zero-order correlation is reversed in the corresponding partial correlation, it indicates that the third variable thereby controlled is a ‘suppressor’ in the relationship between the other two (Cohen et al, 2003). Here, this means that FTC at 24 weeks and PTC at 24 weeks shared systematic variance with each other that was independent of variance shared between FTC at 24 weeks and HDRS at 24 weeks—in fact corresponding to error variance in this relationship (when not statistically controlled in a partial correlation).). By way of comparison, the partial correlation between PTC at 24 weeks and HDRS at 24 weeks after controlling for variance shared with FTC at baseline, r=−0.551, p=0.079, was reduced compared with the zero-order correlation and no longer significant; as was that controlling for variance shared with FTC at 4 weeks, r=−0.560, p=0.073. However, the partial correlation controlling for variance shared with FTC at 24 weeks, r=−0.607, p=0.048, was reduced but remained significant. Together, results show that PTC at 24 weeks shared variance with HDRS at 24 weeks that was independent of predictive associations between FTC at baseline and at 4 weeks with HDRS at 24 weeks.
Percent-Change
Table 4 reports percent-change values for FTC, PTC, and HDRS during three time intervals: the earlier (baseline–4 weeks) and later (4–24 weeks) time intervals, as well as over the course of the entire study (baseline–24 weeks). Percent-change values were calculated according to a standard convention, percent-change=((old value−new value)/old value) × 100. Therefore, positive values indicate percent-decrease and negative values indicate percent-increase. A mixed-model repeated-measures ANOVA was performed on the dependent variable theta cordance percent-change, with time interval (baseline–4 weeks, 4–24 weeks) and location (frontal, posterior) as within-subjects variables and clinical response (responder, non-responder) as a between-subjects variable. The two-way interaction of time interval and clinical response appeared as a credible trend, F(1,10)=4.22, p=0.067, ηp2=0.297, as did the three-way interaction of time interval, location, and clinical response, F(1,10)=4.10, p=0.070, ηp2=0.291 (Supplementary Figure S1, right panel). No other effects approached significance, F<1.
Percent-Change Correlations
Table 5 reports percent-change correlations among FTC, PTC, and HDRS variables. Notably, FTC percent-change over the course of the study (baseline–24 weeks) correlated with HDRS percent-change over the course of the study (baseline–24 weeks), r=−0.601, p=0.039. More robustly and specifically, however, FTC percent-change in the earlier time interval (baseline–4 weeks) predicted HDRS percent-change in the subsequent time interval (4–24 weeks), r=−0.790, p=0.002 (Supplementary Figure S3, left panel); as well as over the course of the study (baseline–24 weeks), r=−0.744, p=0.006 (Supplementary Figure S3, right panel).
To evaluate topographical specificity of results, correlations were re-examined after controlling for variance shared with PTC percent-change (4–24 weeks), in which HDRS percent-change (baseline–24 weeks) was predicted by: (1) FTC percent-change (baseline–24 weeks) and (2) FTC percent-change (baseline–4 weeks). The resulting partial correlation for: (1) was reduced and no longer significant, r=−0.519, p=0.102, and (2) was reduced but remained significant, r=−0.700, p=0.016. Together, results show that the association of FTC percent-change in the earlier time interval (baseline–4 weeks) predicting HDRS percent-change over the course of the study (baseline–24 weeks) was largely independent of variance shared with PTC percent-change in the later time interval (4–24 weeks).
Demographic Characteristics and History
Demographic characteristics and history variables (see again Table 1) were examined as potential alternative explanations for variance in antidepressant response. Of the quantitative variables, none were statistically different between responders and non-responders, p>0.05. However, some showed significant correlations with FTC or HDRS and were therefore examined further. Number of prior depressive episodes was correlated with FTC at baseline, r=0.623, p=0.031. However, the strength of this relationship was found to depend on the presence of one extreme score (40 prior depressive episodes, for a non-responder). When data from this individual were removed, the correlation was no longer significant, r=0.470, p=0.145 (In contrast, with data from this individual removed the zero-order correlation between baseline FTC and 24 weeks HDRS remained significant, r=0.605, p=0.049, if slightly reduced compared with that reported for the full sample. Similarly, all other correlations were duly re-examined after removing data from this individual but results were not substantially altered.).
Furthermore, the correlation between FTC at baseline and HDRS at 24 weeks was re-examined (after removing data from this individual), while controlling for variance shared with number of prior depressive episodes. The partial correlation between FTC at baseline and HDRS at 24 weeks remained significant, r=0.698, p=0.025, and notably, was even larger than the zero-order correlation (Finding a partial correlation that is larger than the original zero-order correlation is another signature of statistical suppression, indicating that the third variable thereby controlled is a ‘suppressor’ in the relationship between the other two (Cohen et al, 2003). Here, this means that number of prior depressive episodes accounted for variance in FTC, which corresponded to error variance in the correlation between FTC and HDRS (when not statistically controlled in a partial correlation). Note that similar evidence for statistical suppression was found for the two following demographic/history variables that were likewise controlled in partial correlations (years of education, age).). Years of education was correlated with HDRS at baseline, r=−0.579, p=0.048. The partial correlation between FTC percent-change (baseline–24 weeks) and HDRS percent-change (baseline–24 weeks), after controlling variance shared with years of education, r=−0.662, p=0.027, was significant, and notably, larger than the zero-order correlation. Similarly, the partial correlation between FTC percent-change (baseline–4 weeks) and HDRS percent-change (baseline–24 weeks), after controlling for variance shared with years of education, r=−0.783, p=0.004, remained significant, and notably, was even larger than the zero-order correlation. Age was correlated with HDRS at 4 weeks, r=−0.651, p=0.022. The partial correlation between FTC percent-change (baseline–4 weeks) and HDRS percent-change (4–24 weeks), after controlling for variance shared with age, r=−0.803, p=0.002, remained significant, and notably, was even larger than the zero-order correlation. Unipolar/bipolar diagnosis showed a possible trend for association with clinical response, χ2=3, p=0.083. However, no correlations (Spearman's rank-order) with FTC or HDRS variables were significant, p>0.05. Together, results show that predictive associations between FTC and HDRS variables were largely independent of variance shared with demographic/history variables including number of prior depressed episodes, years of education, age, or unipolar/bipolar diagnosis.
DISCUSSION
SCC DBS appears to be a promising approach to TRD, but is invasive, costly, and has potential for adverse effects. Therefore, it is important to identify potential biomarkers for predicting antidepressant response to DBS treatment before intervention. This study examined the utility of resting-state FTC at baseline as well as early changes during treatment for predicting antidepressant response to DBS. Two main questions were addressed: (1) would FTC at baseline predict antidepressant response, and (2) would early changes in FTC predict antidepressant response? It was expected that FTC at pre-treatment baseline and FTC changes early after treatment onset would both be predictive of antidepressant response to treatment by SCC DBS. In answer to these questions, it was found that: (1) lower FTC at baseline (and higher FTC at 4 weeks) predicted better antidepressant response at 24 weeks, and (2) early FTC increases (baseline–4 weeks) predicted better antidepressant response subsequently (4–24 weeks) and over the course of the study (baseline–24 weeks).
It is worth emphasizing that FTC was here ‘predictive’ of antidepressant response in two senses of the word: statistical relationship and moreover, temporal precedence. Therefore, it is permissible to suppose that FTC changes might have been part of a causal chain of events linking SCC DBS to subsequent changes in depression severity. In contrast, PTC (at 24 weeks) was concurrently associated with antidepressant response (at 24 weeks), and therefore was only ‘predictive’ of antidepressant response in terms of statistical relationship. Overall, results suggest a picture in which early increases in FTC reflected the initiation of a process of PFC and/or ACC normalization, concurrent with ongoing SCC DBS, which led to subsequent decreases in depression. PTC appeared to be only epiphenomenally related to these events. Mechanisms of DBS are best studied with higher resolution methods and will require extensive modeling techniques of higher density data—analyses that are beyond the scope of this report. Such work will likely will require modeling of network dynamics and not necessarily states of any one region in isolation. Future studies will attempt to correlate concurrently acquired PET and EEG to address these issues.
Given the small sample size and the importance of accurately determining the nature of biomarkers for potential clinical applications, replication of present findings is crucial. Present findings are overall consistent with previous ones in the broadest sense that FTC at pre-treatment baseline and FTC changes from baseline were strongly predictive of subsequent antidepressant response. However, present findings are somewhat discrepant with previous ones at a more detailed level. Specifically, in previous studies in which patients were treated by antidepressant medications, FTC decreases from baseline have predicted better clinical response (Bares et al, 2008, 2010, 2012; Cook et al, 2002; Hunter et al, 2010). Moreover, Bares et al (2012) found higher FTC at baseline for clinical responders compared with non-responders. Similarly, Pizzagalli et al (2001, 2002) and Mulert et al (2007) found that higher theta CSD at pre-treatment baseline localized to rostral ACC predicted better clinical response to antidepressant medications.
In this study, in contrast, it was found that: (1) lower FTC at baseline and (2) early FTC increases from baseline were each associated with better clinical response to SCC DBS. Additional studies will be required to clarify apparent discrepancies between these findings and those previously reported in other depression subgroups treated with various medications. Considering some possible reasons for these apparent discrepancies, it should first be remembered there are many potential neural generators contributing to the present FTC measures, including medial PFC as well as rostral ACC. Moreover, theta activity can be correlated between ACC and PFC (Pizzagalli et al, 2003). It cannot be determined whether present results are due to direct DBS effects at the anatomical target of direct stimulation or somewhere downstream in the distributed limbic–cortical network for mood and affect regulation, which is hypothesized to be dysfunctional in TRD (Mayberg, 2009). If it can be supposed that the present FTC measures reflected substantial contributions from PFC, finding that FTC increases predicted depression decreases would make better sense, and would be moreover consistent with the notion of hypofrontality as a causal mechanism in the etiology and maintenance of major depressive disorder and TRD.
Although the mechanism of action for SCC DBS is not well understood, it would likely be characteristically different from that for the various antidepressant medications that have been examined in previous studies. In this connection, a singular aspect of the present group of patients was that all had previously failed to respond to antidepressant therapies similar to those under investigation in previous reports, as well as ECT. Furthermore, that patients in the present sample were likely atypical as well in terms of disease severity, chronicity, and resistance to treatment. Other characteristics that could distinguish the present sample of patients from those in previous investigations include the facts that patients were all receiving various drug therapies concurrently with DBS, and that patients with unipolar and bipolar depression subtypes were mixed together. However, some of these potential influences were statistically evaluated in this report (number of prior depressive episodes, number of current medications, and unipolar/bipolar diagnosis), and were not found to be strongly impacting the predictive relationships between FTC and antidepressant response. Nevertheless, potential influences from sample characteristics cannot be discounted; therefore independent replications with larger samples are needed.
Additional technical factors may have contributed to these results; however, none seem sufficient to explain the robust individual differences among patients in FTC at baseline and after 4 weeks, or the systematic associations of these with antidepressant response. Possibilities include the following. (1) The electrodes chosen to represent FTC (F3, Fz, and F4) were different from what is typical (Fp1, Fz, and Fp2). However, some previous studies have included F4 (eg, Cook et al, 2009), so the present set of frontal electrodes is mostly overlapping with those in previous studies. (2) DBS was discontinued just before each EEG recording session (and was re-started at the conclusion) to avoid gross stimulation artifact. Therefore, results might have been partially affected by transient changes in SCC/medial PFC activation associated with discontinuation of DBS. However, all patients were exposed to a similar discontinuation protocol and there were no acute changes in behavior or self-report with discontinuation of DBS in any of the patients. (3) Resting-state EEG was recorded with eyes open (to minimize potential drowsiness). This would likely result in less contribution from power in alpha frequencies, and thus could have led to overestimation of relative power in theta frequencies for cordance calculations. (4) Breach rhythms (Cobb et al, 1979) can distort EEG recordings located near a skull defect (because of, eg, injury or craniotomy), showing enhanced power mainly for faster frequency oscillations such as mu and beta (Brigo et al, 2010). Theoretically, breach rhythms could have affected cordance calculations. However, there was little to no remaining opening in the skull from DBS surgery and electrode implantation, as there was a cap placed in the quarter-size burr hole. Any minor skull opening was restricted to parasaggital skull just anterior to the coronal suture, which would not be especially close to focal recording sites for FTC or PTC measures. Moreover, all patients had a standardized surgical procedure with comparably sized burr holes placed in a near identical location. Thus, breach rhythms do not seem sufficient to explain the robust individual differences among patients in FTC at baseline and after 4 weeks DBS, or the systematic associations of these with antidepressant response. Additional studies are needed to better evaluate possible effects on FTC because of DBS surgery and electrode implantation independently of effects of chronic intracranial stimulation.
CONCLUSIONS
FTC at pre-treatment baseline and FTC changes early in treatment both have potential utility as biomarkers for predicting 6-month clinical response to SCC DBS for TRD.
References
Asada H, Fukuda Y, Tsunoda S, Yamaguchi M, Tonoike M (1999). Frontal midline theta rhythms reflect alternative activation of prefrontal cortex and anterior cingulate cortex in humans. Neurosci Lett 274: 29–32.
Bares M, Brunovsky M, Kopecek M, Novak T, Stopkova P, Sos P et al (2008). Early reduction in prefrontal theta QEEG cordance value predicts response to venlafaxine treatment in patients with resistant depressive disorder. Eur Psychiatry 23: 350–355.
Bares M, Brunovsky M, Novak T, Kopacek M, Stopkova P, Sos P et al (2010). The change of prefrontal QEEG theta cordance as a predictor of response to buprion treatment in patients who had failed to respond to previous antidepressant treatments. Eur Neuropsychopharmacol 20: 459–466.
Bares M, Novak T, Brunovsky M, Kopacek M, Stopkova P, Krajca V et al (2012). The change of QEEG prefrontal cordance as a response predictor to antidepressive intervention in bipolar depression. A pilot study. J Psychiatr Res 46: 219–225.
Bewernick BH, Hurlemann R, Matusch A, Kayser S, Grubert C, Hadrysiewicz B et al (2010). Nucleus accumbens deep brain stimulation decreases ratings of depression and anxiety in treatment-resistant depression. Biol Psychiatry 67: 110–116.
Brigo F, Cicero R, Fiaschi A, Bongiovanni LG (2010). The breach rhythm. Clin Neurophysiol 122: 2116–2120.
Cobb WA, Guiloff RJ, Cast J (1979). Breach rhythm: the EEG related to skull defects. Electroencephalogr Clin Neurophysiol 47: 251–271.
Cohen J, Cohen P, West SG, Aiken LS (2003). Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. Lawrence Erlbaum Associates: Mahwah, NJ.
Cook IA, Hunter AM, Abrams M, Siegman B, Leuchter AF (2009). Midline and right frontal brain function as a physiologic biomarker of remission in major depression. Psychiatry Res Neuroimag 174: 152–157.
Cook IA, Leuchter AF, Morgan M, Witte E, Stubbeman WF, Abrams M et al (2002). Early changes in prefrontal activity characterize clinical responders to antidepressants. Neuropsychopharmacology 27: 120–131.
Davidson RJ, Pizzagalli D, Nitschke JB, Putnam K (2002). Depression: perspectives from affective neuroscience. Ann Rev Psychol 53: 545–574.
Hamani C, Mayberg H, Snyder B, Giaccobe P, Kennedy S, Lozano AM (2009). Deep brain stimulation of the subcallosal cingulate gyrus for depression: anatomical location of active contacts in clinical responders and a suggested guideline for targeting. J Neurosurg 111: 1209–1215.
Hamilton MA (1960). Rating scale for depression. J Neurol Neurosurg Psychiatry 23: 56–61.
Hasler G, Northoff G (2011). Discovering imaging endophenotypes for major depression. Mol Psychiatry 16: 604–619.
Holtzheimer PE, Kelley ME, Gross RE, Filkowski, Garlow SJ, Barrocas A et al (2012). Subcallosal cingulate deep brain stimulation for treatment-resistant unipolar and bipolar depression. Arch Gen Psychiatry 69: 150–158.
Hunter AM, Muthen BO, Cook IA, Leuchter AF (2010). Antidepressant response trajectories and quantitative electroencephalography (QEEG) biomarkers in major depressive disorder. J Psychiatr Res 44: 90–98.
Kennedy SH, Giacobbe P, Rizvi SJ, Placenza FM, Nishikawa Y, Mayberg HS et al (2011). Deep brain stimulation for treatment-resistant depression: follow-up after 3 to 6 years. Am J Psychiatry 168: 502–510.
Korb AS, Cook IA, Hunter AM, Leuchter AF (2008). Brain electrical source differences between depressed subjects and healthy controls. Brain Topogr 21: 138–146.
Knyazev GG (2007). Motivation, emotion, and their inhibitory control mirrored in brain oscillations. Neurosci Biobehav Rev 31: 377–395.
Kringelbach ML, Jenkinson N, Owen SLF, Aziz TZ (2007). Translational principles of deep brain stimulation. Nat Rev Neurosci 8: 623–635.
Leuchter AF, Cook IA (2010). Reply to Kuo and Tsai. Psychiatry Res 180: 61–62.
Leuchter AF, Cook IA, Lufkin RB, Dunkin J, Newton TF, Cummings JL et al (1994). Cordance: a new method for assessment of cerebral perfusion and metabolism using quantitative electroencephalography. NeuroImage 1: 208–219.
Lozano AM, Mayberg HS, Giacobbe P, Hamani C, Craddock RC, Kennedy SH (2008). Subcallosal cingulate gyrus deep brain stimulation for treatment-resistant depression. Biol Psychiatry 64: 461–467.
Malone Jr DA, Dougherty DD, Rezai AR, Carpenter LL, Friehes GM, Eskandar EN et al (2009). Deep brain stimulation of the ventral capsule/ventral striatum for treatment-resistant depression. Biol Psychiatry 65: 267–275.
Mayberg HS (1997). Limbic-cortical dysregulation: a proposed model of depression. J Neuropsychiatry 9: 471–481.
Mayberg HS (2009). Targeted electrode-based modulation of neural circuits for depression. J Clin Invest 119: 717–725.
Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C et al (2005). Deep brain stimulation for treatment-resistant depression. Neuron 45: 651–660.
Mulert C, Juckel G, Brunnmeier M, Karch S, Leicht G, Mergl R et al (2007). Prediction of treatment response in major depression: integration of concepts. J Affect Disord 98: 215–225.
Pizzagalli D, Pascual-Marqui RD, Nitschke JB, Oakes TR, Larson CL, Abercrombie HC et al (2001). Anterior cingulate activity as a predictor of degree of treatment response in major depression: evidence from brain electrical tomography analysis. Am J Psychiatry 158: 405–415.
Pizzagalli DA, Hendrick AM, Horras KA, Davidson RJ (2002). Anterior cingulate theta activity is associated with degree of treatment response in major depression. Int Congress Ser 1232: 711–717.
Pizzagalli DA, Oakes TR, Davidson RJ (2003). Coupling of theta activity and glucose metabolism in the human rostral anterior cingulate cortex: an EEG/PET study of normal and depressed subjects. Psychophysiology 40: 939–949.
Price JL, Drevets WC (2010). Neurocircuitry of mood disorders. Neuropsychopharmacology 35: 192–216.
Price JL, Drevets WC (2012). Neural circuits underlying the pathophysiology of mood disorders. Trends Cognitive Sci 16: 61–71.
Sauseng P, Griesmayr B, Freunberger R, Klimesch W (2010). Control mechanisms in working memory: a possible function of EEG theta oscillations. Neurosci Biobehav Rev 34: 1015–1022.
Sauseng P, Klimesch W (2008). What does phase information of oscillatory brain activity tell us about cognitive processes? Neurosci Biobehav Rev 32: 1001–1013.
Acknowledgements
This study was funded by grants from the Dana Foundation (HSM), Stanley Medical Research Institute (HSM), Woodruff Foundation (HSM), Emory Healthcare (HSM), and K23 MH077869 (PEH). Devices were donated by Advanced Neuromodulation Systems/St Jude Medical Neuromodulation. We thank Andrea Barrocas, Megan Filkowski, and Margaret Craighead for assistance with patient coordination. In addition, the authors would like to thank Alex Alverson for assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Mr Broadway, Mr Hilimire, Dr Parks, Mr DeVylder, and Dr Corballis declare no conflict of interest. Dr Holtzheimer has received grant funding from the Greenwall Foundation, NARSAD, National Institutes of Health Loan Repayment Program, NIMH, and Northstar; he has received consulting fees from AvaCat Consulting, St Jude Medical and Oppenheimer. Dr Mayberg has a consulting agreement with St Jude Medical, which has licensed her intellectual property to develop SCC DBS for the treatment of severe depression (US 2005/0033379A1). The terms of these arrangements have been reviewed and approved by Emory University in accordance with their conflict of interest policies. Dr Mayberg has current grant funding from the Dana Foundation, NARSAD, National Institute of Mental Health (NIMH), Stanley Medical Research Institute, and Woodruff Foundation.
Additional information
Supplementary Information accompanies the paper on the Neuropsychopharmacology website
Rights and permissions
About this article
Cite this article
Broadway, J., Holtzheimer, P., Hilimire, M. et al. Frontal Theta Cordance Predicts 6-Month Antidepressant Response to Subcallosal Cingulate Deep Brain Stimulation for Treatment-Resistant Depression: A Pilot Study. Neuropsychopharmacol 37, 1764–1772 (2012). https://doi.org/10.1038/npp.2012.23
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2012.23
Keywords
This article is cited by
-
Deep brain stimulation for refractory major depressive disorder: a comprehensive review
Molecular Psychiatry (2024)
-
Opportunities and challenges for the use of deep brain stimulation in the treatment of refractory major depression
Discover Mental Health (2024)
-
Effects of deep brain stimulation on cognitive functioning in treatment-resistant depression: a systematic review and meta-analysis
Molecular Psychiatry (2023)
-
Brain-wide changes in excitation-inhibition balance of major depressive disorder: a systematic review of topographic patterns of GABA- and glutamatergic alterations
Molecular Psychiatry (2023)
-
Hormonal regulation of circuit function: sex, systems and depression
Biology of Sex Differences (2019)