Abstract
Autoimmune diseases are frequently characterized by the presence of autoantibodies directed against nucleic acid-protein complexes present in the nucleus of the cell. The mechanisms by which these autoantigenic molecules escape immunological tolerance are largely unknown, although a number of recent observations suggest that modified self-proteins generated during apoptosis may play an important role in the development of autoimmunity. It has been hypothesized that the recognition of these modified self-proteins by the immune system may promote autoantibody production. While apoptosis is specifically characterized by posttranslational modification of proteins, recent findings also show that nucleic acids are modified. This review summarizes the specific cleavages of some of these key nucleic acids, i.e. chromosomal DNA, ribosomal RNA and small structural RNAs (U1 snRNA, Y RNA), in apoptotic cells. Cell Death and Differentiation (2000) 7, 616–627
Similar content being viewed by others
Immunological tolerance broken by autoantigen modifications?
Systemic autoimmunity is characterized by the production of autoantibodies which are directed toward a number of autoantigenic proteins. Expression of these autoantigens can be either ubiquitous, as in non-organ-specific autoimmune diseases, or restricted to a particular type of cell, as in organ-specific autoimmune diseases. It is still not understood which driving force propels self-proteins to escape immunological tolerance and thus to become autoantigenic. Several hypotheses have been formulated of which the ‘unusual modification of self-proteins’ has received increasing attention during the last 5–6 years.
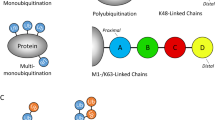
The ‘unusual modification of self-proteins’ hypothesis implies that when control of a normal cellular process (e.g. apoptosis) is lost, novel or neo-epitopes may be uncovered or generated on self-proteins and presented to the immune system as non-self (Figure 1A). Such novel or neo-epitopes might be the result of a change in 3D-structure as a consequence of a proteolytic cleavage or an amino acid modification. The presentation of the neo-epitope by Th-cells might lead to an immune reaction, which in certain cases, due to ‘intramolecular/intermolecular epitope spreading’, could explode into the production of a broad range of autoantibodies directed to the whole self-antigen. The process of epitope spreading in relation to autoantibody production has been extensively reviewed by others and will be touched on only briefly here.1,2 As shown in Figure 1B, an autoimmune response is elicited by the presentation of a T-cell neo-epitope, e.g. a modification of self-component C1, by antigen-presenting cells. This activates a population of autoreactive Th-cells that have the capacity to induce B-cells carrying the C1 neo-epitope to proliferate and mature. Autoreactive B-cells carrying antigen receptors specific for individual components of the ‘C1/C2/C3-complex’ (see Figure 1B), will all be able to present the specific ‘T-cell C1 neo-epitope’ as well as C2 and C3 (neo-)epitopes. Thus, these B-cells, with different antigen receptor specificities, can be induced to proliferate and mature by a single Th-cell population specific for only one neo-epitope.
Generation of novel/neo-epitopes during apoptotic cell death and possible consequences. (A) Massive apoptosis and/or an inefficient/defective clearance of apoptotic cells can result in an accumulation of antigenic epitopes that are exposed to the immune system. The subsequent presentation of apoptotically modified molecules will initiate an immune reaction, which in certain cases, due to ‘epitope spreading’, could evolve into the production of a broad range of autoantibodies directed to the whole (non-modified) self-component. (B) Intra- and intermolecular epitope spreading. B-cells with various specificities for the same molecule (intramolecular), or for other tightly associated molecules (intermolecular) can be stimulated by T-cells specific for one neo-epitope. See text for further details
A typical example of a process in which many self-proteins are cleaved or modified is apoptosis,3,4 a genetically determined program that eliminates unneeded, senescent, or damaged cells. It has been shown that autoantigens targeted in SLE become concentrated in two discrete populations of surface structures on apoptotic cells, namely apoptotic bodies and apoptotic surface blebs.5,6,7 Under normal conditions such unwanted apoptotic cells are quickly and efficiently removed by macrophages or other phagocytic cells without ever being exposed to the immune system. However, when the clearance of apoptotic cell remnants is for some reason less efficient this might result in a temporarily increased exposure of modified self-components to the immune system. Genetic and/or environmental factors may then contribute to activation of the immune system. Interestingly, impaired phagocytosis of apoptotic cells in SLE patients has been observed.8 Genetic factors may be critical determinants in the subsequent development of an autoimmune disease.4 Unregulated, excessive or massive apoptosis, for example induced by viral or bacterial infections, or following exposure to toxins, drugs or UV-light, might, possibly in combination with defective clearance, also result in activation of the immune system (Figure 1A). Although experimental data to support the latter pathway are still very scarce, it has been reported that SLE patients contain increased levels of circulating apoptotic cells.9,10
Modifications of autoantigenic proteins
The best characterized apoptotically induced modification is the specific cleavage of autoantigenic proteins by cysteinyl aspartate-specific proteinases (caspases).11 At present, the apoptotic cleavage by caspases of many autoantigens has been documented (reviewed in12). Interestingly, many autoantigens that are not cleaved by caspases were recently found to be cleaved by granzyme B.13,14 Granzyme B is a serine protease present in the cytoplasmic granules of cytotoxic T-lymphocytes (CTLs) and natural killer (NK) cells and induces, in the presence of perforin, apoptosis.15,16,17 Since most of the reported apoptotically cleaved autoantigens have important functions in the cell, their cleavage during early stages of apoptosis is likely to interfere with basic cellular processes.
Although caspase-mediated cleavage of autoantigens has been the most studied to date, other types of posttranslational modifications which occur during apoptosis and which might play a role in the generation of autoantibodies have been described. It has been shown recently that at least four SR (serine arginine-rich) proteins, i.e. pp54, pp42, pp34, and pp23, become hyperphosphorylated and associated with the U1 snRNP complex in apoptotic cells.18 Rutjes and co-workers19 reported recently on the specific dephosphorylation of the La (SS-B) autoantigenic protein during apoptosis. Crosslinking by tissue transglutaminase,20 (de)ubiquitina-tion,21 citrullination,22 and poly(ADP-ribosyl)ation are also modifications that may create novel epitopes or increase the half-life of autoantigenic proteins present in apoptotic cells, leading to changes in the exposure of these modified antigens to the immune system (also reviewed elsewhere in this issue, and in12).
In addition to the extensive modification of proteins during apoptosis, also nucleic acids, DNA and some selected RNAs, are cleaved during this process. Remarkably, most of these modified nucleic acids are known autoantigens, i.e. autoimmune patients make autoantibodies against these molecules, or these nucleic acids are tightly associated with autoantigenic protein components. Anti-nucleic acid autoantibodies most likely arise via intermolecular epitope spreading (see Figure 1B). In case of an RNA-protein complex, a B-cell might express an antigen receptor that recognizes (a modification of) the RNA component, e.g. component C3 of the C1/C2/C3-complex in Figure 1B. After internalization and processing of the RNA-protein complex via the RNA-specific B-cell, a variety of different epitopes, including the C1 neo-epitope, will be presented on the B-cell. Exposure of the C1 neo-epitope on the B-cell results in its stimulation via the C1 neo-epitope specific Th-cell and the subsequent production of anti-RNA antibodies.
Modification of chromosomal DNA
The nucleosome as antigen in SLE
Eukaryotic DNA is organized as chromatin, a compact structure composed of a string of subunits, the so-called nucleosomes. A nucleosome contains a protein core with DNA wound around its surface like thread around a spool. The protein core is an octamer containing two copies each of histones H2A (14 kDa), H2B (13.8 kDa), H3 (15.3 kDa) and H4 (1.3 kDa). Each nucleosome is associated with one molecule of histone H1 (23 kDa). The DNA content of a single nucleosome plus the DNA linking neighboring nucleosomes varies between 160 and 200 nucleotides. It has been shown that DNA circulating in the blood is always in a nucleosomal form,23,24 and that systemic lupus erythematosus (SLE) patients produce autoantibodies directed to nucleosomes.25 It is generally accepted that among these autoantibodies also reactivities directed to DNA and/or histones are present.26
Chromosomal DNA is cleaved by a caspase-dependent endonuclease in apoptotic cells
Cell death by apoptosis, first described by Kerr and co-workers,27 plays a crucial role during the development, proliferation and differentiation of mammalian organisms. This process is characterized morphologically by condensation and fragmentation of nuclei and cells, and biochemically by the fragmentation of chromosomal DNA into nucleosomal units (∼200 bp).28
In 1998 Enari and co-workers29 reported the isolation and characterization of a protein that induces DNA degradation in isolated nuclei of normal non-apoptotic murine cells after treatment with caspase-3, suggesting that these cells carry an inactive form of that particular nuclease. As caspase-3 treatment was necessary to activate this endonuclease, it was designated CAD (caspase-activated DNase). In the cytosol of growing non-apoptotic murine cells, Enari and co-workers also discovered the protein that inhibited the activity of CAD. This protein, which they called ICAD (inhibitor of CAD), is associated with CAD in a cytoplasmic complex, the DNA fragmentation factor (DFF). Caspase-3 activation in apoptotic cells results in the cleavage of ICAD thereby releasing active CAD. Since CAD contains a nuclear localization signal, it translocates to the nucleus where it cleaves chromosomal DNA.29,30 In humans, DFF is composed of a 45 kDa subunit (DFF45) that is homologous to murine ICAD, and a 40 kDa subunit (DFF40), also known as CPAN (caspase-activated nuclease), that is homologous to murine CAD.29,30,31,32,33,34 In this review we will only use the ICAD and CAD annotations.
The DFF complex unraveled
CAD is present in healthy cells where it is held in an inactive state through the association with its inhibitor ICAD. The ICAD protein is inactivated in apoptotic cells via caspase-3 cleavage thereby releasing CAD, which subsequently cleaves chromosomal DNA. Upon apoptotic stimulation in vitro (e.g. with recombinant caspase-3 or apoptotic cell lysates) and in vivo, ICAD (331 aa) is cleaved into three different protein fragments of 10–15 kDa due to the presence of two caspase-3 cleavage sites, i.e. 114DETD117 and 221DAVD224 (Figure 2A).30,32 The finding that ICAD can also be cleaved in caspase-3 knockout cells suggested that other caspases may also cleave ICAD.35 Indeed, it has been shown recently that ICAD can be efficiently cleaved (in vitro) and inactivated by caspase-3 and caspase-7, weakly by caspase-8 and not by caspase-6.36
Schematic map of ICAD and CAD. (A) Schematic ICAD protein organization. The capacity of individual ICAD subfragments to bind, inhibit, or act as a chaperone with respect to CAD is indicated on the right, and is based on several studies.37,38,39 DETD/DAVD, caspase-3 cleavage sites;30,32 +, strong activity; +/−, poor activity. (B) Schematic CAD protein domain organization. The CAD protein contains an activator (or regulator) domain that activates the endonuclease activity that is localized in the catalytic domain.38,40 D1, D2 and D3, refer to the ICAD fragments in (A). See text for further details
Several studies have addressed the protein domains of ICAD and CAD that interact with each other. The truncated ICAD proteins D1 (aa 1–117), D2 (aa 118–224), D3 (aa 225–331), D1-2 (aa 1–224) and D2-3 (aa 118–331),37,38 were generated based on the locations of the caspase cleavage sites (Figure 2A).32 It was shown that domains D1-2 and D2-3 of the ICAD protein bind more stably to CAD than the single domains D1, D2, or D3.38 Fine mapping revealed that (i) D1 binds to the first 80 amino acids of CAD; (ii) D2 appears to bind to a region between amino acids 117 and 150; and (iii) D3 is likely to bind to a region between residues 81 and 117.36 Because the most important function of ICAD is to inhibit the function of CAD, the relationship between the binding of the individual ICAD domains and the activity of CAD was investigated. The activity of CAD could be effectively inhibited by the D1-2 and D2-3 domains.37 D1, D2, and D3 were much less efficient inhibitors of CAD activity which correlates with their low binding capacity. Gu and co-workers39 mapped the CAD binding domain of ICAD to amino acid residues 101–180, and the inhibitory domain necessary to inhibit the activity of CAD to amino acid residues 23–100. Based on the three published CAD binding domains of ICAD, i.e. amino acids 1–224,37 118–33137 and 101–180,39 the most important amino acid residues for CAD binding are likely to be located between amino acid residues 101 and 180 in ICAD. However, the finding of Gu and co-workers39 that the inhibitory domain is located between amino acid residues 23 and 100 contradicts the results of McCarty and co-workers37,38 who demonstrated that the site was contained between amino acid residues 1–224 and 118–331. Further experiments will be required to clarify this issue.
As a consequence of alternative splicing, two isoforms of ICAD are generated, the short ICAD-S/DFF35 (comprising 265 and 268 aa in the murine and human protein, respectively) and the long ICAD-L/DFF45 (both 331 aa).29,30,39 Although both proteins bind to CAD, only ICAD-L/DFF45 has chaperone activity to assist in the correct folding of CAD during synthesis. This indicated that the most C-terminal region of ICAD-L/DFF45 (aa 265–331) is important for its chaperone-like function.39 However, McCarty and co-workers37 reported that D1 (aa 1–117) contains a chaperone-like function and that D1-2 (aa 1–224) has only poor chaperone activity. These results indicate that there are two putative chaperone-like domains, one located in the N-terminal half and the other in the C-terminal half of ICAD.
A comparable mapping of the CAD protein domains has also been performed (Figure 2B).40 Deletion of the C-terminal catalytic domain (aa 162–345) abrogated the endonuclease activity of CAD (345 aa) but not its binding activity to ICAD. Removal of amino acid residues 1–83, which include the regulatory or activator domain, produced a CAD mutant that was constitutively active and was neither bound to ICAD nor required caspase-3 for activation. The regulatory or activator domain (aa 1–83) of CAD and the D1 domain (aa 1–117) of ICAD are homologous to each other and to the regulatory CIDE-N domain of pro-apoptotic CIDE (cell death-inducing DFF45-like effector) proteins.39,41 Mutational analysis of the most conserved amino acid residues within the regulatory CIDE-N domain of CAD showed that this domain is not only involved in the association with ICAD, but also promotes the activity of the endonuclease or catalytic domain (aa 162–345). This has also been suggested by the studies of McCarty and co-workers.38 Although the CIDE-N domains of CAD and ICAD are homologous, their functions are certainly not identical. The CIDE-N domain of ICAD inhibits the endonuclease activity of CAD, whereas the CIDE-N domain of CAD enhances the endonuclease activity.39,40 Differences in function of the CIDE-N domains might result from differences in amino acid sequence or from conformational differences in the respective proteins. This issue may be solved by the analysis of chimeric ICAD and CAD proteins in which the CIDE-N domains have been swapped.
The DFF complex during apoptosis
In healthy cells, CAD is inactive as a consequence of its association with ICAD.37,38,39,40 During apoptosis the ICAD protein is cleaved at amino acid residues 117 and 224 which results in the abrogation of its inhibitory activity and release of CAD.32 Released and thus activated CAD translocates to the nucleus and cleaves chromosomal DNA. It has been shown that CAD exhibits nuclease activity on protein-free DNA in the presence of caspase-3 and ICAD.29,31,33 However, the finding that CAD showed weaker endonuclease activity on naked DNA than chromosomal DNA from intact nuclei,32 suggested that other nuclear factors are necessary for optimal CAD activity. These factors appeared to be the abundant chromatin-associated proteins histone H1,36 HMG-1 (high mobility group protein 1)31 and HMG-2.42 Remarkably, in apoptotic cells expressing caspase-resistant ICAD, chromosomal DNA is not cleaved although chromatin is condensed.43 This pointed to the presence of a caspase-activated but ICAD-independent factor involved in the condensation of chromatin. Recently, the protein involved in this process, Acinus (apoptotic chromatin condensation inducer in the nucleus), has been cloned. The Acinus protein is activated during apoptosis by caspase-3 and induces chromatin condensation without DNA fragmentation.44 The mechanism by which Acinus induces chromatin condensation has not yet been described.
Modification of ribosomal RNA
The 60S large ribosomal subunit as antigen in SLE
In cells of higher eukaryotes the 60S large ribosomal subunit, which contains the 5S (121 nts), 5.8S (159 nts) and 28S (approx. 5000 nts) ribosomal RNA (rRNA) molecules, and the 40S small ribosomal subunit, which contains the 18S (approx. 2000 nts) rRNA molecule, associate into the 80S ribosomal complex during translation. Whereas the small 40S subunit binds to messenger RNA (mRNA), the large 60S subunit catalyzes the peptide-bond formation. More than 80 proteins are associated with the rRNA components of the 80S ribosome, and some of them are autoantigenic.
The major autoantigenic proteins of the eukaryotic 80S ribosomal complex recognized by autoantibodies from sera of SLE patients are the P (phospho) proteins P0 (37 kDa), P1 (19 kDa) and P2 (17 kDa).45 The P proteins are associated with the 60S ribosomal subunit as a pentameric complex (one copy of P0, and two copies of P1 and P2 each) via direct binding to the 28S rRNA molecule.46 RNase protection studies indicated that the pentameric P protein complex protects nucleotides 1838–1936 of the 28S rRNA molecule suggesting that this part of the RNA contains the protein binding site.47 In addition to the anti-P antibodies, sera of SLE patients may also contain antibodies directed to the 28S rRNA molecule itself.48,49 The autoantigenic region of the 28S rRNA molecule, also referred to as 28S-Ag RNA, has been mapped between nucleotides 1944–2002 and is thus in close proximity to the binding site of the pentameric P complex.49 The P proteins and the 28S-Ag RNA together form a functional GTPase domain. Autoantibodies against the ribosomal S10 (20 kDa),50 L12 (20 kDa)51 and L7 (30 kDa)52 proteins have also been detected but modifications of these proteins have not yet been reported.
The 28S rRNA molecule is cleaved during apoptosis
The 28S rRNA molecule consists of conserved and variable or so-called divergent domains (D1–D12),53 of which the conserved domains constitute the core RNA backbone of the ribosome. The presence of divergent domains (D) in 28S rRNA of higher eukaryotes is the result of evolutionary large-scale expansions, both in length and diversity, in regions that are inserted between the conserved domains.54,55 As a result, nearly half of the 28S rRNA sequences in eukaryotes consists of divergent RNA.56 Although the precise function of D domains is unknown, the fact that certain subdomains, i.e. D2c and D8b, diverge faster during phylogeny than one might expect from random mutations as compared to other D domains, seems to indicate that they have more than a structural role to play.56,57 D domains have therefore been suggested to be involved in the translational machinery as riboregulators, protein anchoring regions, or as domains for RNA-RNA interactions.58
In 1993, 17 years after the discovery that chromosomal DNA is cleaved during apoptosis,28 Houge and co-workers observed that in apoptotic rat myeloid leukemia IPC-81 cells the 28S rRNA molecule, which is a component of the 60S large ribosomal subunit, was cleaved into several distinct fragments.59 Cleavage of 28S rRNA was first observed between 2 and 4 h after the induction of apoptosis and correlated with an increase in the percentage of morphologically changed (apoptotic) cells. The autoantigenic ribosomal P proteins are not susceptible to apoptotic cleavage by caspases60 or granzyme B.14 Houge and co-workers have studied the behavior of the 28S rRNA during apoptosis in parallel with the degradation of chromosomal DNA and other markers of apoptosis.59,61,62 Although their initial results indicated that cleavage of 28S rRNA coincided with DNA fragmentation,59,61 they recently demonstrated that the cleavage of 28S rRNA and chromosomal DNA may occur independently.62 The 28S rRNA molecule is also cleaved in the apoptotic human leukemia cell lines K562, Molt-3, Molt-4 and U937.62 However, in the human HL-60 leukemia cells apoptosis could be induced without any signs of rRNA cleavage. Houge and co-workers observed no specific cleavage of 18S rRNA during apoptosis.59,61,62 However, recent reports revealed that both the 28S rRNA and the 18S rRNA are cleaved in several cell lines during apoptosis.63 Interestingly, it has also been reported that the mitochondrial 16S rRNA molecule can be cleaved after apoptotic stimulation.64
The apoptotic cleavage sites in rat 28S rRNA have been mapped to the two largest divergent domains, D2 (approx. nts 400–1200) and D8 (approx. nts 2700–3400),61 each of which contains two apoptotic cleavage sites. The two apoptotic cleavage sites in the 5′-region of 28S rRNA, i.e. divergent domain D2 (D2c), have been mapped at about nucleotide 890 and between nucleotides A1192-U1193 (Figure 3A). In divergent domain D8 (D8b), which is in the 3′-half of 28S rRNA, the two apoptotic cleavage sites are between nucleotides U3257-U3258, and U3288 to U3290 (Figure 3B).61 The observed cleavage patterns in the hypervariable55,57 D2 and D8 subdomains, D2c and D8b, are apoptosis-specific because necrosis induction and the incubation with several RNases (RNase T1 and RNase U2) resulted in different cleavage patterns.61 Based on the speculation that the primary target that is cleaved in the 28S rRNA molecule can either be in the D2 or in the D8 domain, it was hypothesized that there might be two alternative apoptotic cleavage pathways.58 In pathway 1, apoptotic cleavage starts in D8b and is subsequently followed by a secondary cleavage in D2c. Pathway 2 is characterized by an initial cleavage 5′ upstream of the D2c subdomain followed by a 3′ cleavage downstream of the D2c subdomain which results in the excision of D2c.58 In apoptotic bovine endothelial cells the alternative targets for rRNA cleavage are the D6 and D8 domains.61 Cleavage in D8 is speculated to be mediated by an RNase activity that is activated during apoptosis because D8 is, in comparison to D2 and D6, more sensitive to the incubation with RNase T1 and RNase U2.58,61 A detailed characterization of the apoptotic 28S rRNA cleavage products in human cells has not yet been published.
Modification of the 28S rRNA molecule during apoptosis. Schematic secondary structure of the 5′-half (A) and 3′-half (B) of 28S rRNA in combination with the 5.8S rRNA (A). The apoptotic cleavage sites, as they occur in the D2c and D8b subdomains of the rat 28S rRNA sequence, are indicated by arrows.61 The gray shaded box marks the region containing the binding site of the P proteins and the immunodominant region as reported for the human 28S rRNA molecule.47,49 The positions of the divergent domains D1-D12 are indicated. The secondary structure used to create this figure was obtained from the ‘RNA Secondary Structures’ website (http://pundit.icmb.utexas.edu/). Note that due to the lack of an available structure of rat 28S rRNA the corresponding mouse structure was used. The highlighted D2 and D8 sequence elements (containing the apoptotic cleavage sites) correspond to the rat sequence
Possible consequences of ribosomal RNA cleavage
Ribosomal RNA (28S) can be added to the growing list of (marker) molecules known to be modified during the apoptotic process. As both 18S rRNA and 28S rRNA are constituents of the 80S ribosomal complex that is involved in the translation of mRNAs, it is tempting to speculate that cleavage of ribosomal RNAs may contribute to the inhibition of protein synthesis. However, as cleavage of the ribosomal RNAs seems in certain cases to be a cell-specific event,62 the mechanism of rRNA cleavage can also be considered as a non-specific event that reflects the generalized shut down of translation and homeostatic regulation during caspase regulated cell death.
Modifications of messenger RNA
Because ribosomal RNAs are cleaved during apoptosis, one might also expect some apoptosis-specific cleavage of mRNA molecules. However, only a few reports have described an increased rate of mRNA turnover during apoptosis.65,66 It is likely that an increased rate of mRNA degradation in apoptotic cells is due to the activation of the nucleolytic activities that are described in the other paragraphs of this review. However, in view of the extensive structural heterogeneity of mRNAs, their generally short half lives, and the abrogation of their synthesis (both transcription and processing) and translation during apoptosis, it would not be surprising that a special machinery for apoptotic mRNA degradation is absent from eukaryotic cells.
Modifications of small structural RNAs
The U1 snRNP complex as autoantigen in SLE
During splicing non-coding or intron sequences are removed from precursor mRNA (pre-mRNA) molecules in order to obtain functional mature mRNA.67 The first and triggering step in this process is the association of the U1 small nuclear ribonucleoprotein (U1 snRNP) complex with the 5′-splice site of an exon. This snRNP complex consists of the U1 snRNA molecule (165 nts) and the U1 snRNP specific proteins U1A, U1C, and U1-70K plus a set of eight proteins, called the Sm proteins, which are shared with other U snRNPs. Most of the individual protein components of the U1 snRNP complex are targeted by autoantibodies present in the serum of patients with SLE and SLE-overlap syndromes (reviewed in68). During apoptosis, the U1-70K protein is specifically cleaved leading to the appearance of a 40 kDa fragment,69,70 whereas the U1A, U1C and Sm-B/B′ proteins are not detectably modified.60,71 All proteins remain associated with the U1 snRNP complex in apoptotic cells.71
The U1 snRNA molecule itself is a major target of autoimmunity in SLE-overlap syndromes,72 and it has been shown that changes in the titer of anti-U1 snRNA autoantibodies may correlate with the severity of the disease.73 The most immunodominant epitopes of the autoantigenic U1 snRNA molecule are located in stemloop II (nts 49–65 and 76–90) and stemloop IV (nts 150–153),74 and were recently characterized in more detail using several recombinant human monoclonal antibodies (scFvs).75,76
The U1 snRNA molecule is cleaved during apoptosis
The fate of the U1 snRNA molecule during apoptosis was examined by polyacrylamide gel electrophoresis and Northern hybridization. In all tested apoptotic mammalian cell lines (Jurkat, human T cell leukemia; HeLa, human cervix carcinoma; HL-60, human promyelocytic leukemia; 4B1, mouse cells overexpressing the human Fas-receptor), U1 snRNA was specifically cleaved.71 Cleavage of U1 snRNA appeared to be a universal phenomenon, as this snRNA was cleaved in various cell types rendered apoptotic with a variety of stimuli (anti-Fas mAb 7C11, murine Fas-ligand, anisomycin, staurosporine, cycloheximide). Intriguingly, the non-autoantigenic U2, U3, U4, U5 and U6 snRNA molecules were not detectably modified. The truncated U1 snRNA molecules migrate as a doublet in denaturing polyacrylamide gels, which is the result of cleavages occurring at the 5′-side of either ψ6 or ψ7 in the single-stranded 5′-end of the snRNA (Figure 4A).71 This might suggest that two flanking pseudouridines (ψ) are involved in the selection of cleavage sites. However, the U2 snRNA molecule is not cleaved despite the presence of a similar ψ-doublet in a single-stranded region near the 5′-end (nucleotides 7 and 8).77 These data suggest that other structural elements are also necessary for cleavage to occur.
Modifications of the autoantigenic U1 snRNP and Ro RNP complexes during apoptosis. (A) Modifications of the U1 snRNP complex. During apoptosis the U1-70K protein is cleaved by caspase-3 into a 40-kDa fragment that remains associated with the U1 snRNP complex. Furthermore, U1 snRNA is cleaved near the 5′-end of the molecule at two flanking pseudouridines (ψ)71 (see box for details; arrows indicate cleavage sites). (B) Modifications of the Ro RNP complex. Apoptosis results in the dephosphorylation and partial cleavage of the La protein. Furthermore, the otherwise stable hY RNA component, in this case hY1 RNA, is rapidly cleaved/degraded (see box for details; although the exact borders of the resulting hY RNA fragments are not known yet, they are likely to be located in the region marked by the arrows). All modifications are indicated by scissors. See text for further details
The Ro RNP complex as antigen in SLE and SjS
Another prominent autoantigenic RNA-protein complex is the Ro RNP complex. Ro RNPs are small cytoplasmic RNA-protein complexes which contain the 50 kDa La (SS-B) protein and the 60 kDa Ro protein (Ro60). The autoantigenic Ro and La proteins were initially identified by autoantibodies present in the sera from patients with SLE and Sjögren's syndrome (SjS).78 In contrast to the well characterized function of U snRNP complexes, the function of Ro RNP complexes is still unknown. The RNA backbone of Ro RNP complexes is a Y RNA molecule, of which four have been identified in humans: hY1 (112 nts), hY3 (101 nts), hY4 (93 nts) and hY5 (84 nts).79 The hY RNA molecules, which are all RNA polymerase III transcripts, are characterized by an oligouridylate stretch at the 3′-end to which the La protein is bound and a conserved stem structure formed by extensive base-pairing between the evolutionarily conserved 5′ and 3′ ends, which is the binding site of Ro60.79 In contrast to the protein components of the Ro RNP complex, autoantibodies recognizing hY RNAs are restricted to hY5 RNA.80
It has been shown recently that La is cleaved by granzyme B,14 and that the protein is rapidly dephosphorylated and partly cleaved during apoptosis.19 The Ro60 protein is not detectably modified by caspases or granzyme B (references14,60 and our own unpublished results).
The hY RNAs are cleaved/degraded during apoptosis
Upon exposure of all cell types tested to a variety of apoptotic stimuli the small cytoplasmic hY RNAs are extensively, rapidly and selectively cleaved/degraded during apoptosis (Figure 4B).81 In contrast, other RNA polymerase III products like 7SL RNA, 5S rRNA and tRNA are not detectably cleaved. The length of the various hY RNA cleavage/degradation products was determined by co-immunoprecipitation, which showed that the apoptotic fragments that remain associated with Ro60 range from 22 to 36 nucleotides, while those that remain associated with the La protein range from 27 to 36 nucleotides. This heterogeneity in size is due to (i) the fact that the fragments are derived from 4 RNAs (hY1, hY3, hY4 and hY5); (ii) the 3′-end heterogeneity of native individual hY RNAs; and (iii) the presence of both 5′-end and 3′-end fragments of these RNAs as the Ro60 binding site is composed of a hybrid of these. The size of the apoptotic hY RNA cleavage/degradation products implies that these do not result from a single endonucleolytic cleavage reaction. Either several endonucleolytic cleavages or a combination of endo- and exonuclease activities are required to generate these products.
The apoptotic modifications of U1 snRNA and hY RNA are caspase-dependent
To determine whether the activation of caspases is required to induce apoptotic cleavage of U1 snRNA and cleavage/degradation of hY RNA, Jurkat cells were cultured in the presence of four cell permeable tetrapeptide caspase inhibitors, Ac-YVAD-CMK, Z-DEVD-FMK, Z-IETD-FMK, or Z-LEHD-FMK (irreversible inhibitors of caspases 1, 3, 8 and 9, respectively), prior to and during apoptosis induction.71,81 Cleavage of U1 snRNA was partly inhibited in the presence of the caspase-1, -3 and -8 inhibitors, but not by the caspase-9 inhibitor. These results indicated that U1 snRNA cleavage is dependent on caspase activation, and that a caspase-activated RNase (CAR) might be involved in this event.71
The cleavage/degradation of the hY RNA molecules was almost completely inhibited in the presence of the caspase-1, -3 and -8 inhibitors, which suggests that this process is also dependent on CAR.81 In contrast, the caspase-9 inhibitor only partially inhibited hY RNA cleavage/degradation. It thus seems that hY RNA cleavage/degradation is mediated by the activation of caspase-8 and the subsequent activation of an effector caspase, e.g. caspase-1 or caspase-3, that is responsible for the activation of the ribonuclease.
Possible consequences of small structural RNA cleavage
The removal of the first 5–6 nucleotides including the 2,2,7-trimethylguanosine-cap (TMG) of U1 snRNA may have several consequences. The most obvious of these is that pre-mRNA splicing would be inhibited since the formation of a commitment complex at the 5′ exon/intron junction, to which the U1 snRNA molecule binds via its 5′-end, may be thwarted. Previously, it has been shown that oligonucleotides complementary to the first 14 nucleotides of the U1 snRNA molecule can block pre-spliceosome and spliceosome assembly in vitro.82 Alternatively, cleavage of U1 snRNA may change the specificity of pre-mRNA splicing. This possibility is supported by some recent observations. First, hyperphosphorylated SR proteins, which have been shown to be involved in alternative splice site selection, become associated with the U1 snRNP complex during apoptosis.18 Second, it has been demonstrated that purified phosphorylated SR proteins can restore in vitro splicing activity in extracts depleted of U1 snRNP, suggesting that the U1 snRNP complex may not be essential for this process.83 Therefore, it is tempting to speculate that SR proteins may substitute for the modified components of U1 snRNP, i.e. U1-70K and U1 snRNA. This may be associated with the alternative splicing of mRNAs encoding apoptosis regulating factors such as bcl-x, Ich-1, or IEX-1, all of which exist in pro-apoptotic or anti-apoptotic isoforms that are regulated at the level of pre-mRNA splicing (reviewed in12). In fact, it has recently been shown that overexpression of an SR protein can regulate the splice site selection of the mRNA encoding Ich-1.84
As the function of the Ro RNP complexes is still unknown, it is difficult to speculate about the implications that cleavage/degradation of hY RNA molecules during apoptosis might have on cellular processes. The apoptotic modification of key proteins which are involved in important cellular processes, like cell cycle regulation, signaling, DNA repair, cell homeostasis or cell survival, will certainly contribute to the irreversibility of the apoptotic process. This might also be true for the hY RNAs, as they have recently been suggested to be involved in the translational control of ribosomal protein mRNAs and possibly other 5′TOP (terminal oligopyrimidine-containing) mRNAs.85 The rapid, specific and efficient cleavage/degradation of hY RNAs during apoptosis suggests that these molecules have an as yet unknown key function in the cell.
Concluding remarks
The mechanism(s) by which autoantigens escape immunological tolerance are largely unknown. However, recent observations, such as the impaired phagocytosis of apoptotic cells in SLE patients,18 suggest that modified self-proteins (autoantigens) generated during apoptosis or necrosis, may play a role in the development of autoimmunity. As such, also the study of unusual modifications of RNA molecules, i.e. 28S rRNA, U1 snRNA and hY RNAs, rather than proteins during apoptosis is important and opens a complete new field of research. The enzymatic activity responsible for the cleavage of 28S rRNA, U1 snRNA and hY RNAs, is the first indication for the existence of caspase-activated ribonucleases (CARs). The fact that CAR only affects the autoantigenic U1 snRNA and not the non-autoantigenic U2, U3, U4, U5 or U6 snRNAs is intriguing. The same holds for the Y RNAs which are, as far as we know, the only RNA polymerase III products that are cleaved/degraded during apoptosis.
The modified nucleic acids which have been summarized in this review are all known autoantigenic molecules or associated with autoantigenic proteins. Their modification during apoptosis suggests a certain degree of selectivity because other small structural RNAs are not cleaved. In this respect it will be important to isolate and characterize the caspase-activated RNase or CAR that must be responsible for the cleavage of these RNA molecules.
Abbreviations
- Ac:
-
acetyl
- aa:
-
amino acid
- CAD:
-
caspase-activated DNase
- CAR:
-
caspase-activated RNase
- CMK:
-
chloromethylketone
- CPAN:
-
caspase-activated nuclease
- DFF:
-
DNA fragmentation factor
- FMK:
-
fluoromethylketone
- ICAD:
-
inhibitor of CAD
- mRNA:
-
messenger RNA
- nts:
-
nucleotides
- pre-mRNA:
-
precursor mRNA
- rRNA:
-
ribosomal RNA
- scFv:
-
single chain variable fragment
- SLE:
-
systemic lupus erythematosus
- snRNA:
-
small nuclear RNA
- snRNP:
-
small nuclear ribonucleoprotein
- SR protein:
-
serine arginine-rich protein
- SjS:
-
Sjögren's syndrome
- tRNA:
-
transfer RNA
- ψ:
-
pseudouridine
- TMG:
-
2,2,7-trimethylguanosine
- Z:
-
benzyloxycarbonyl
References
Craft J and Fatenejad S . (1997) Self antigens and epitope spreading in systemic autoimmunity. Arthritis Rheum. 40: 1374–1382
McCluskey J, Farris AD, Keech CL, Purcell AW, Rischmueller M, Kinoshita G, Reynolds P and Gordon TP . (1998) Determinant spreading: lessons from animal models and human disease. Immunol. Rev. 164: 209–229
Vaishnaw AK, McNally JD and Elkon KB . (1997) Apoptosis in the rheumatic diseases. Arthritis Rheum. 40: 1917–1927
Rosen A and Casciola-Rosen LA . (1999) Autoantigens as substrates for apoptotic proteases: implications for the pathogenesis of systemic autoimmune disease. Cell Death Differ. 6: 6–12
Casciola-Rosen LA, Anhalt GJ and Rosen A . (1994) Autoantigens targeted in systemic lupus erythematosus are clustered in two populations of surface structures on apoptotic keratinocytes. J. Exp. Med. 179: 1317–1330
Casciola-Rosen LA, Anhalt GJ and Rosen A . (1995) DNA-dependent protein kinase is one of a subset of autoantigens specifically cleaved early during apoptosis. J. Exp. Med. 182: 1625–1634
Casciola-Rosen LA, Rosen A, Petri M and Schlissel M . (1996) Surface blebs on apoptotic cells are sites of enhanced procoagulant activity: implications for coagulation events and antigenic spread in systemic lupus erythematosus. Proc. Natl. Acad. Sci. USA 93: 1624–1629
Herrmann M, Voll RE, Zoller OM, Hagenhofer M, Ponner BB and Kalden JR . (1998) Impaired phagocytosis of apoptotic cell material by monocyte-derived macrophages from patients with systemic lupus erythematosus. Arthritis Rheum. 41: 1241–1250
Emlen W, Niebur J and Kadera R . (1994) Accelerated in vitro apoptosis of lymphocytes from patients with systemic lupus erythematosus. J. Immunol. 152: 3685–3692
Courtney PA, Crockard AD, Williamson K, Irvine AE, Kennedy RJ and Bell AL . (1999) Increased apoptotic peripheral blood neutrophils in systemic lupus erythematosus: relations with disease activity, antibodies to double stranded DNA, and neutropenia. Ann. Rheum. Dis. 58: 309–314
Cohen GM . (1997) Caspases: the executioners of apoptosis. Biochem. J. 326: 1–16
Utz PJ and Anderson P . (1998) Posttranslational protein modifications, apoptosis, and the bypass of tolerance to autoantigens. Arthritis Rheum. 41: 1152–1160
Andrade F, Roy S, Nicholson D, Thornberry N, Rosen A and Casciola-Rosen LA . (1998) Granzyme B directly and efficiently cleaves several downstream caspase substrates: implications for CTL-induced apoptosis. Immunity 8: 451–460
Casciola-Rosen LA, Andrade F, Ulanet D, Wong WB and Rosen A . (1999) Cleavage by granzyme B is strongly predictive of autoantigen status: Implications for initiation of autoimmunity. J. Exp. Med. 190: 815–825
Shi L, Kam CM, Powers JC, Aebersold R and Greenberg AH . (1992) Purification of three cytotoxic lymphocyte granule serine proteases that induce apoptosis through distinct substrate and target cell interactions. J. Exp. Med. 176: 1521–1529
Shresta S, Macivor DM, Heusel JW, Russell JH and Ley TJ . (1995) Natural killer and lymphokine-activated killer cells require granzyme B for the rapid induction of apoptosis in susceptible target cells. Proc. Natl. Acad. Sci. USA 92: 5679–5683
Heusel JW, Wesselschmidt RL, Shresta S, Russell JH and Ley TJ . (1994) Cytotoxic lymphocytes require granzyme B for the rapid induction of DNA fragmentation and apoptosis in allogeneic target cells. Cell 76: 977–987
Utz PJ, Hottelet M, van Venrooij WJ and Anderson P . (1998) Association of phosphorylated serine/arginine (SR) splicing factors with the U1-small ribonucleoprotein (snRNP) autoantigen complex accompanies apoptotic cell death. J. Exp. Med. 187: 547–560
Rutjes SA, Utz PJ, Broekhuis C, van der Heijden A, van Venrooij WJ and Pruijn GJ . (1999) The La (SS-B) autoantigen, a key protein in RNA biogenesis, is dephosphorylated and cleaved early during apoptosis. Cell Death Differ. 6: 976–986
Piacentini M and Colizzi V . (1999) Tissue transglutaminase: apoptosis versus autoimmunity. Immunol. Today 20: 130–134
Marushige Y and Marushige K . (1995) Disappearance of ubiquitinated histone H2A during chromatin condensation in TGF beta 1-induced apoptosis. Anticancer Res. 15: 267–272
Asaga H, Yamada M and Senshu T . (1998) Selective deimination of vimentin in calcium ionophore-induced apoptosis of mouse peritoneal macrophages. Biochem. Biophys. Res. Commun. 243: 641–646
Rumore PM and Steinman CR . (1990) Endogenous circulating DNA in systemic lupus erythematosus. Occurrence as multimeric complexes bound to histone. J. Clin. Invest. 86: 69–74
Rumore PM, Muralidhar B, Lin M, Lai C and Steinman CR . (1992) Haemodialysis as a model for studying endogenous plasma DNA: oligonucleosome-like structure and clearance. Clin. Exp. Immunol. 90: 56–62
Losman MJ, Fasy TM, Novick KE and Monestier M . (1992) Monoclonal autoantibodies to subnucleosomes from a MRL/Mp(−)+/+ mouse. Oligoclonality of the antibody response and recognition of a determinant composed of histones H2A, H2B, and DNA. J. Immunol. 148: 1561–1569
Tax WJ, Kramers C, van-Bruggen MC and Berden JH . (1995) Apoptosis, nucleosomes, and nephritis in systemic lupus erythematosus. Kidney Int. 48: 666–673
Kerr JF, Wyllie AH and Currie AR . (1972) Apoptosis: a basic biological phenomenon with wide-ranging implications in tissue kinetics. Br. J. Cancer 26: 239–257
Wyllie AH, Kerr JF and Currie AR . (1980) Cell death: the significance of apoptosis. Int. Rev. Cytol. 68: 251–306
Enari M, Sakahira H, Yokoyama H, Okawa K, Iwamatsu A and Nagata S . (1998) A caspase-activated DNase that degrades DNA during apoptosis, and its inhibitor ICAD. Nature 391: 43–50
Sakahira H, Enari M and Nagata S . (1998) Cleavage of CAD inhibitor in CAD activation and DNA degradation during apoptosis. Nature 391: 96–99
Liu X, Li P, Widlak P, Zou H, Luo X, Garrard WT and Wang X . (1998) The 40-kDa subunit of DNA fragmentation factor induces DNA fragmentation and chromatin condensation during apoptosis. Proc. Natl. Acad. Sci. USA 95: 8461–8466
Liu X, Zou H, Slaughter C and Wang X . (1997) DFF, a heterodimeric protein that functions downstream of caspase-3 to trigger DNA fragmentation during apoptosis. Cell 89: 175–184
Halenbeck R, MacDonald H, Roulston A, Chen TT, Conroy L and Williams LT . (1998) CPAN, a human nuclease regulated by the caspase-sensitive inhibitor DFF45. Curr. Biol. 8: 537–540
Mukae N, Enari M, Sakahira H, Fukuda Y, Inazawa J, Toh H and Nagata S . (1998) Molecular cloning and characterization of human caspase-activated DNase. Proc. Natl. Acad. Sci. USA 95: 9123–9128
Tang D and Kidd VJ . (1998) Cleavage of DFF-45/ICAD by multiple caspases is essential for its function during apoptosis. J. Biol. Chem. 273: 28549–28552
Liu X, Zou H, Widlak P, Garrard W and Wang X . (1999) Activation of the apoptotic endonuclease DFF40 (caspase-activated DNase or nuclease). Oligomerization and direct interaction with histone H1. J. Biol. Chem. 274: 13836–13840
McCarty JS, Toh SY and Li P . (1999) Study of DFF45 in its role of chaperone and inhibitor: Two independent inhibitory domains of DFF40 nuclease activity. Biochem. Biophys. Res. Commun. 264: 176–180
McCarty JS, Toh SH and Li P . (1999) Multiple domains of DFF45 bind synergistically to DFF40: Roles of caspase cleavage and sequestration of activator domain of DFF40. Biochem. Biophys. Res. Commun. 264: 181–185
Gu J, Dong RP, Zhang C, McLaughlin DF, Wu MX and Schlossman SF . (1999) Functional interaction of DFF35 and DFF45 with caspase-activated DNA fragmentation nuclease DFF40. J. Biol. Chem. 274: 20759–20762
Inohara N, Koseki T, Chen S, Benedict MA and Nunez G . (1999) Identification of regulatory and catalytic domains in the apoptosis nuclease DFF40/CAD. J. Biol. Chem. 274: 270–274
Inohara N, Koseki T, Chen S, Wu X and Nunez G . (1998) CIDE, a novel family of cell death activators with homology to the 45 kDa subunit of the DNA fragmentation factor. EMBO J. 17: 2526–2533
Toh SY, Wang XD and Li P . (1998) Identification of the nuclear factor HMG2 as an activator for DFF nuclease activity. Biochem. Biophys. Res. Commun. 250: 598–601
Sakahira H, Enari M, Ohsawa Y, Uchiyama Y and Nagata S . (1999) Apoptotic nuclear morphological change without DNA fragmentation. Curr. Biol. 9: 543–546
Sahara S, Aoto M, Eguchi Y, Imamoto N, Yoneda Y and Tsujimoto Y . (1999) Acinus is a caspase-3-activated protein required for apoptotic chromatin condensation. Nature 401: 168–173
Elkon KB, Parnassa AP and Foster CL . (1985) Lupus autoantibodies target ribosomal P proteins. J. Exp. Med. 162: 459–471
Uchiumi T, Wahba AJ and Traut RR . (1987) Topography and stoichiometry of acidic proteins in large ribosomal subunits from Artemia salina as determined by crosslinking. Proc. Natl. Acad. Sci. USA 84: 5580–5584
Uchiumi T and Kominami R . (1992) Direct evidence for interaction of the conserved GTPase domain with 28 S RNA with mammalian ribosomal acidic phosphoproteins and L12. J. Biol. Chem. 267: 19179–19185
Uchiumi T, Traut RR, Elkon K and Kominami R . (1991) A human autoantibody specific for a unique conserved region of 28 S ribosomal RNA inhibits the interaction of elongation factors 1 alpha and 2 with ribosomes. J. Biol. Chem. 266: 2054–2062
Chu JL, Brot N, Weissbach H and Elkon K . (1991) Lupus antiribosomal P antisera contain antibodies to a small fragment of 28S rRNA located in the proposed ribosomal GTPase center. J. Exp. Med. 174: 507–514
Bonfa E, Parnassa AP, Rhoads DD, Roufa DJ, Wool IG and Elkon KB . (1989) Antiribosomal S10 antibodies in humans and MRL/lpr mice with systemic lupus erythematosus. Arthritis Rheum. 32: 1252–1261
Sato T, Uchiumi T, Kominami R and Arakawa M . (1990) Autoantibodies specific for the 20-KDa ribosomal large subunit protein L12. Biochem. Biophys. Res. Commun. 172: 496–502
von Mikecz A, Hemmerich P, Peter HH and Krawinkel U . (1994) Characterization of eukaryotic protein L7 as a novel autoantigen which frequently elicits an immune response in patients suffering from systemic autoimmune disease. Immunobiology 192: 137–154
Michot B, Hassouna N and Bachellerie JP . (1984) Secondary structure of mouse 28S rRNA and general model for the folding of the large rRNA in eukaryotes. Nucleic Acids Res. 12: 4259–4279
Raue HA, Klootwijk J and Musters W . (1988) Evolutionary conservation of structure and function of high molecular weight ribosomal RNA. Prog. Biophys. Mol. Biol. 51: 77–129
Michot B and Bachellerie JP . (1987) Comparisons of large subunit rRNAs reveal some eukaryote-specific elements of secondary structure. Biochimie 69: 11–23
Gutell RR and Fox GE . (1988) A compilation of large subunit RNA sequences presented in a structural format. Nucleic Acids Res. 16: (Suppl) r175–r269
Gonzalez IL, Gorski JL, Campen TJ, Dorney DJ, Erickson JM, Sylvester JE and Schmickel RD . (1985) Variation among human 28S ribosomal RNA genes. Proc. Natl. Acad. Sci. USA 82: 7666–7670
Houge G and Doskeland SO . (1996) Divergence towards a dead end? Cleavage of the divergent domains of ribosomal RNA in apoptosis. Experientia 52: 963–967
Houge G, Doskeland SO, Boe R and Lanotte M . (1993) Selective cleavage of 28S rRNA variable regions V3 and V13 in myeloid leukemia cell apoptosis. FEBS Lett. 315: 16–20
Casiano CA, Martin SJ, Green DR and Tan EM . (1996) Selective cleavage of nuclear autoantigens during CD95 (Fas/APO-1)-mediated T cell apoptosis. J. Exp. Med. 184: 765–770
Houge G, Robaye B, Eikhom TS, Golstein J, Mellgren G, Gjertsen BT, Lanotte M and Doskeland SO . (1995) Fine mapping of 28S rRNA sites specifically cleaved in cells undergoing apoptosis. Mol. Cell Biol. 15: 2051–2062
Samali A, Gilje B, Doskeland SO, Cotter TG and Houge G . (1997) The ability to cleave 28S ribosomal RNA during apoptosis is a cell-dependent trait unrelated to DNA fragmentation. Cell Death Differ. 4: 289–293
Lafarga M, Lerga A, Andres MA, Polanco JI, Calle E and Berciano MT . (1997) Apoptosis induced by methylazoxymethanol in developing rat cerebellum: organization of the cell nucleus and its relationship to DNA and rRNA degradation. Cell Tissue Res. 289: 25–38
Crawford DR, Lauzon RJ, Wang Y, Mazurkiewicz JE, Schools GP and Davies KJ . (1997) 16S mitochondrial ribosomal RNA degradation is associated with apoptosis. Free Radic. Biol. Med. 22: 1295–1300
Mondino A and Jenkins MK . (1995) Accumulation of sequence-specific RNA-binding proteins in the cytosol of activated T cells undergoing RNA degradation and apoptosis. J. Biol. Chem. 270: 26593–26601
Owens GP and Cohen JJ . (1992) Identification of genes involved in programmed cell death. Cancer Metastasis Rev. 11: 149–156
Sharp PA . (1994) Split genes and RNA splicing. Cell 77: 805–815
Klein Gunnewiek JM, van de Putte LB and van Venrooij WJ . (1997) The U1 snRNP complex: an autoantigen in connective tissue diseases. An update. Clin. Exp. Rheumatol. 15: 549–560
Casciola-Rosen LA, Miller DK, Anhalt GJ and Rosen A . (1994) Specific cleavage of the 70-kDa protein component of the U1 small nuclear ribonucleoprotein is a characteristic biochemical feature of apoptotic cell death. J. Biol. Chem. 269: 30757–30760
Casciola-Rosen LA, Nicholson DW, Chong T, Rowan KR, Thornberry NA, Miller DK and Rosen A . (1996) Apopain/CPP32 cleaves proteins that are essential for cellular repair: a fundamental principle of apoptotic death. J. Exp. Med. 183: 1957–1964
Degen WGJ, van Aarssen Y, Pruijn GJM, Utz PJ and van Venrooij WJ . (2000) The fate of U1 snRNP during anti-Fas induced apoptosis: specific cleavage of the U1 snRNA molecule. Cell Death Differ. 7: 70–80
van Venrooij WJ, Hoet R, Castrop J, Hageman B, Mattaj IW and van de Putte LB . (1990) Anti-(U1) small nuclear RNA antibodies in anti-small nuclear ribonucleoprotein sera from patients with connective tissue diseases. J. Clin. Invest. 86: 2154–2160
Hoet RMA, Koornneef I, de Rooij DJ, van de Putte LB and van Venrooij WJ . (1992) Changes in anti-U1 RNA antibody levels correlate with disease activity in patients with systemic lupus erythematosus overlap syndrome. Arthritis Rheum. 35: 1202–1210
Hoet RMA, De Weerd P, Klein Gunnewiek J, Koornneef I and van Venrooij WJ . (1992) Epitope regions on U1 small nuclear RNA recognized by anti-U1RNA-specific autoantibodies. J. Clin. Invest. 90: 1753–1762
Teunissen SW, Stassen MH, Pruijn GJ, van Venrooij WJ and Hoet RM . (1998) Characterization of an anti-RNA recombinant autoantibody fragment (scFv) isolated from a phage display library and detailed analysis of its binding site on U1 snRNA. RNA 4: 1124–1133
Hoet RMA, Pieffers M, Stassen MH, Raats JMH, de Wildt R, Pruijn GJM, van den Hoogen F and van Venrooij WJ . (1999) The importance of the light chain for the epitope specificity of human anti-U1 small nuclear RNA autoantibodies present in systemic lupus erythematosus patients. J. Immunol. 163: 3304–3312
Massenet S, Mougin A and Branlant C . (1998) Posttranscriptional modifications in the U small nuclear RNAs. In Modification and editing of RNA. Grosjean H and Benne R eds, (ASM Press) pp. 201–227
Tan EM . (1989) Antinuclear antibodies: diagnostic markers for autoimmune diseases and probes for cell biology. Adv. Immunol. 44: 93–152
van Venrooij WJ, Slobbe RL and Pruijn GJ . (1993) Structure and function of La and Ro RNPs. Mol. Biol. Rep. 18: 113–119
Boulanger C, Chabot B, Menard HA and Boire G . (1995) Autoantibodies in human anti-Ro sera specifically recognize deproteinized hY5 Ro RNA. Clin. Exp. Immunol. 99: 29–36
Rutjes SA, van der Heijden A, Utz PJ, van Venrooij WJ and Pruijn GJ . (1999) Rapid nucleolytic degradation of the small cytoplasmic Y RNAs during apoptosis. J. Biol. Chem. 274: 24799–24807
Temsamani J, Agrawal S and Pederson T . (1991) Biotinylated antisense methylphosphonate oligodeoxynucleotides. Inhibition of spliceosome assembly and affinity selection of U1 and U2 small nuclear RNPs. J. Biol. Chem. 266: 468–472
Crispino JD, Blencowe BJ and Sharp PA . (1994) Complementation by SR proteins of pre-mRNA splicing reactions depleted of U1 snRNP. Science 265: 1866–1869
Jiang ZH, Zhang WJ, Rao Y and Wu JY . (1998) Regulation of Ich-1 pre-mRNA alternative splicing and apoptosis by mammalian splicing factors. Proc. Natl. Acad. Sci. USA 95: 9155–9160
Pellizzoni L, Lotti F, Rutjes SA and Pierandrei AP . (1998) Involvement of the Xenopus laevis Ro60 autoantigen in the alternative interaction of La and CNBP proteins with the 5′ UTR of L4 ribosomal protein mRNA. J. Mol. Biol. 281: 593–608
Acknowledgements
The authors thank PJ Utz (Stanford, CA, USA) and MJ Clemens (London, UK) for critical reading of the manuscript. We thank Future Diagnostics BV (Wijchen, The Netherlands) for financial support to WGJ Degen. The work of WJ van Venrooij and GJM Pruijn was supported in part by the Netherlands Foundation for Chemical Research (SON) with financial aid from the Netherlands Organization for Scientific Research (NWO) and the Dutch Technology Foundation (STW). JMH Raats is a research fellow of the Royal Netherlands Academy of Arts and Sciences (KNAW).
Author information
Authors and Affiliations
Corresponding author
Additional information
Edited by M Piacentini
Rights and permissions
About this article
Cite this article
Degen, W., Pruijn, G., Raats, J. et al. Caspase-dependent cleavage of nucleic acids. Cell Death Differ 7, 616–627 (2000). https://doi.org/10.1038/sj.cdd.4400672
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cdd.4400672
Keywords
This article is cited by
-
Artichoke extracts in cancer therapy: do the extraction conditions affect the anticancer activity?
Future Journal of Pharmaceutical Sciences (2020)
-
Novel ethanocycloheptono [3,4,5-kl]benzo[a]xanthene induces apoptosis in BEL-7402 cells
Molecular and Cellular Biochemistry (2018)
-
Thioredoxin/thioredoxin reductase system involvement in cerebellar granule cell apoptosis
Apoptosis (2014)
-
Juglanthraquinone C, a novel natural compound derived from Juglans mandshurica Maxim, induces S phase arrest and apoptosis in HepG2 cells
Apoptosis (2012)
-
Caspase-mediated cleavage of the U snRNP-associated Sm-F protein during apoptosis
Cell Death & Differentiation (2003)