Abstract
Study design: Prospective study on magnetic resonance imaging (MRI) and radiographic findings of the cervical spine.
Objective: To elucidate the age-related changes of the cervical spinal cord and the cervical spinal canal and the relationship between the spinal cord and the spinal canal in asymptomatic subjects using MRI and radiography.
Setting: Tokyo, Japan.
Methods: The transverse area of the cervical spinal cord and the ratio of the anteroposterior diameter to the transverse diameter (RAPT) were investigated, using MRI in 229 asymptomatic subjects. The sagittal spinal canal diameter and anteroposterior diameter of the cervical vertebral body were also measured on plain lateral radiographs. The canal body ratio (CBR), which was defined as the diameter of the spinal canal divided by that of the vertebral body, was calculated.
Results: The transverse spinal cord area correlated negatively with age. RAPT did not correlate with age. The CBR correlated negatively with age. The correlation between spinal cord area and CBR was significant but weak and the correlation between RAPT and CBR was not significant.
Conclusion: The transverse area of the cervical spinal cord measured by MRI decreased with age, while RAPT remained unchanged. The bony spinal canal became narrower with age. The spinal cord area and the shapes of the spinal cord were independent from the spinal canal diameter in asymptomatic subjects. These facts should be considered when evaluating radiological findings in patients with cervical spinal disorders.
Similar content being viewed by others
Introduction
In the treatment of cervical spinal disorders such as compressive myelopathy and spinal cord injury, the transverse area of the cervical spinal cord of the patient has been considered as an effective predictor of clinical outcomes. Several authors have reported that the decreased spinal cord area before decompressive surgery would indicate poor surgical outcomes.1,2,3,4 The evaluation of the spinal cord area should be made after its comparison with norms obtained from asymptomatic subjects of each age group, since it may change with aging just as the cerebrum decreases in size with aging in the elderly. The relationship between the spinal cord and the spinal canal in asymptomatic subjects should also be considered in the treatment of cervical spinal disorders, because patients with a tight spinal canal are more susceptible to spinal cord damage. To date, however, few studies have been made that focused on age-related changes in the cervical spinal cord and cervical spinal canal. The recent development of MRI has made it possible to obtain clear images of the cervical spinal cord non-invasively, thereby making measurements of transverse spinal cord area more applicable to routine practice. This morphometric study was undertaken to clarify age-related changes in the cervical spinal cord and the cervical spinal canal using MRI and radiography in order to establish the basis for the morphometric evaluation of the patients with cervical spinal cord disorders.
Materials and methods
Subjects
Two hundred and twenty-nine Japanese volunteers (118 males and 111 females), who had no past history of cervical spinal disease or trauma, and had no neck, shoulder or arm symptoms, were enrolled in this study. Informed consent was obtained from all subjects prior to their enrollment. The volunteers were recruited via oral advertisement by members of the study team.5 The ages of the subjects were uniformly distributed within a range of 11 to 72 years, and the number of males or females in each decade from teenagers to more than 60 years of age ranged from 15 to 20.
MR imaging
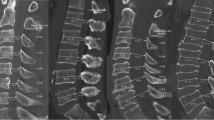
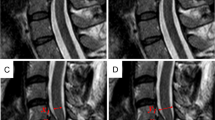
All subjects underwent MRI of the cervical spine using a 0.5 Tesla scanner with a surface neck coil (Resona, Yokogawa medical system, Tokyo). T1 weighted axial images were obtained using a spin echo sequence (TE; 500, TR; 25, FOV; 22 cm, slice thickness; 5 mm, NEX; 2). The slices were made at the mid-vertebral body levels from C3 to C6 as well as at the intervertebral levels from C3–4 to C5–6. The slice planes were set parallel to each intervertebral disc space. Hard copies of the MR images were photographed with a digital camera (Nikon E2N, Tokyo, matrix size 1,300,000), and the images were analyzed on a personal computer (Aptiva H65, IBM Japan, Tokyo) using custom-made measurement software for which accuracy had been proven to be high by our preliminary tests. The transverse area and anteroposterior and transverse diameters of the spinal cord were measured, and the ratio of an anteroposterior to transverse diameters of the spinal cord was calculated (RAPT) (Figure 1). All measurements were performed three times by one of the investigators (M Ishikawa) and the data were averaged.
Radiography
All subjects also underwent lateral radiograph with their neck in the neutral position. They were told to look straight ahead in the relaxed position by an X-ray technician. The focus-film distance was set to 1.5 meters. Sagittal spinal canal diameter and anterioposterior diameter of the cervical vertebral body at the mid-vertebral bodies from C3 to C6 were measured. The canal body ratio (CBR) was given by dividing the diameter of the spinal canal by that of the vertebral body to assess the tightness of the spinal canal, and also to eliminate the magnification effect of radiographs.
Evaluation of measurement errors
Errors during measurements and data processing were assessed. First, to determine the difference between true and measured values, the diameter and area of a metal disc with known values were measured and compared. Inter- and intra-observer errors were evaluated as follows. The MR images of two males and two females were randomly selected from each age group (24 subjects in total), and two spine surgeons (M Ishikawa and M Matsumoto) measured the spinal cord area at the C4–5 level and C5 level three times each to evaluate inter-observer errors. The measurements were repeated one month later to evaluate intra-observer errors.
Statistical analyses
Statistical analyses were performed using a ‘Statview 4.5’ (Abacus Concepts, Int., Berkeley). Correlation between the spinal cord area and RAPT with age, height and body weight of the subjects were evaluated using Pearson correlation coefficient. ANOVA was used to evaluate the differences in the transverse area and RAPT among different age groups, while the paired t-test was used to evaluate inter- and intra-observer errors. P values less than 0.05 were considered significant.
Results
Evaluation of measurement errors
The mean area of the metal disc measured by the software was 337.99±1.67 mm2, which was 97.6% of the real size. The coefficient variable was 0.49%. Regarding inter- and intra-observer errors, there was no significant difference in measured values between the two observers (P=0.094 at C4–5, P=0.081 at C5) or between the two measurements performed at separate times by a single observer (P=0.318 at C4–5, P=0.227 at C5).
Spinal cord area
The mean transverse area of the spinal cord was largest at the C4 vertebral level in both males and females, for each age group. Generally, the transverse area was largest in subjects in their twenties and it decreased with age. Males had significantly larger spinal cord areas than females in all age groups except teenagers. The mean transverse areas at C4 in males and females were 91.8±9.7 mm2 and 95.2±8.0 mm2 in teenagers, 100.7±9.7 mm2 and 98.7±9.6 mm2 in those in their twenties, 99.0±7.8 mm2 and 91.1±10.0 mm2 in those in their forties, and 86.4±9.1 mm2 and 85.1±8.3 mm2 in those older than 60 years of age respectively (Figures 2 and 3). The correlation coefficients between spinal cord area and age after twenties, at each level, ranged from −0.23 at C3–4 to −0.47 at C5–6 in males and from −0.31 at C6 to −0.47 at C3 in females. The spinal cord area correlated negatively with age in both males and females (P<0.05).
The correlation coefficients between spinal cord area and height at each level were between 0.28 and 0.55 in males and between 0.24 and 0.27 in females, and the spinal cord areas was correlated positively with height both in males and females (P<0.05). The correlation coefficients between spinal cord area and body weight at each level were between 0.03 and 0.19 in males and between 0.01 and 0.09 in females (statistically not significant).
RAPT
The mean RAPT was smallest at the C5–6 intervertebral level and largest at the C3 vertebral level in males and females of any age groups. The mean RAPT at the C5–6 intervertebral level in males and females were 55.6±4.6% and 54.4±4.4% in teenagers, 54.6±3.9% and 55.2±3.9% in those in their twenties, 55.5±3.7% and 54.3±3.7% in those in their forties and 53.5±3.4% and 54.7±5.2% in those older than 60 years of age respectively. There was no significant gender difference in RAPT. The correlation coefficients between RAPT and age, height, and body weight, at each level, ranged between −0.17 and 0.19 in males and between −0.16 and 0.10 in females (statistically not significant).
Canal Body Ratio (CBR)
The mean CBR in males and females were 0.82±0.20 and 0.90±0.12 at C3 vertebral level, 0.82±0.20 and 0.91±0.13 at C4 vertebral level, 0.86±0.18 and 0.95±0.15 at C5 vertebral level, 0.86±0.18 and 0.95±0.13 at C6 vertebral level respectively (Figure 4).
The correlation coefficients between CBR and age ranged from −0.57 to −0.64 in males, and from −0.23 to −0.42 at each level in females (P<0.05). The CBR significantly decreased with age in both gender. The correlation coefficients between CBR and the transverse area of the spinal cord ranged from 0.02 to 0.12 in males, and from 0.25 to 0.39 in females at each level. The CBR had weak or no correlation with the transverse area of the spinal cord.
Discussion
There have been several studies on the transverse area and RAPT of the spinal cord measured on MR images.6,7,8,9,10 Sherman et al. found no correlation between spinal cord area and age, gender or body weight.6 Tanaka and Tanida reported spinal cord area to have no correlation with age.10,11 Suzuki et al.9 reported spinal cord area to correlate negatively with age but positively with height. The results of these studies are not consistent, partly because the number of subjects was small and the age distribution was not uniform. In the present study, the number of the subjects was sufficiently large for statistical analyses and the age and gender distribution of the subjects were almost equal among each age group. Moreover, the measurement methods were validated by the evaluation of possible errors.
As a result, we found that transverse spinal cord area correlated negatively with age and positively with height but not with body weight. RAPT did not correlate with age. This means that the cervical spinal cord decreases in size with aging while maintaining its shape. The decrease in transverse area of the spinal cord with aging may be attributable to age-related atrophy of the spinal cord or to the differences in body size between young and aged populations, although further study is needed to clarify these issues.
The spinal cord area at each level was smaller in teenagers than the twenties, although the difference was not statistically significant. It is believed that the spinal cord reaches maturity in early childhood, however, subtle growth of the spinal cord may occur in adolescence. This should be investigated by further study that is focused on pediatric population.
Sherman et al. showed that in his study the average spinal cord area at C4 in normal subjects was 121.8 mm2.6 In the present study, the average spinal cord area at C4 in normal subjects was 94.6 mm2. The large difference in the spinal cord area between the two studies may be related not only to pulse sequence in MRI, but also to racial difference in the height of the subjects, since height is positively correlated with the spinal cord area, as shown in this study.
Although MRI has enabled us to evaluate the cervical spinal cord area non-invasively, we must be cautious in interpreting the data obtained, since the values of the spinal cord area may depend on the pulse sequences utilized. Miyasaka performed a basic study in which spinal cord area was measured.12 He found measured spinal cord area to be larger on T1 weighted images and smaller on T2 weighed axial images than the actual size of the spinal cord and attributed this to the data truncation effect which arises at the boundary of the spinal cord and cerebrospinal fluid during the Fourier transformation process.13,14,15 He also found that, on T1 weighted images, the spinal cord area was close to the real value if the window level was set to the average MR values of the spinal cord and cerebrospinal fluid. Suzuki et al.9 studied the reliability of MR measurement of the spinal cord. They scanned and measured a formalin-fixed cadaveric spinal cord and found that measurements made on T1-weighted MR images yielded nearly the same values as the actual spinal cord. Based on these previous studies, we used T1 weighted images to make our measurements.
Wolf stated the decreased sagittal spinal canal diameter would be one cause of the compressive myelopathy,16 and measuring the sagittal spinal canal diameter is widely accepted for one diagnosing method of the compressive myelopathy.17,18 CBR, which eliminates the magnification effect or radiographs, is a good alternative to measurement of the sagittal spinal canal diameter.19 In this study, CBR significantly decreased with age, and this may suggest the bony cervical spinal canal would be narrower with aging even in asymptomatic subjects. The results of this study showed that the correlation between spinal cord area and CBR and between RAPT and CBR were not statistically significant. These findings indicate that the spinal cord area and the shapes of the spinal cord are independent of the spinal canal diameter in asymptomatic subjects of any age groups. This may suggest that an individual with a narrow spinal canal does not always have a small or flat spinal cord. Therefore, patients with negative balance of the spinal cord and the spinal canal do exist, and they may possibly be subject to spinal cord compression.
In summary, the transverse area of the cervical spinal cord area measured on MRI decreased with age, while RAPT remained unchanged. The bony spinal canal would be narrower with age. But there was no significant correlation between the transverse area and the bony spinal canal diameter. These facts should be considered in evaluation of radiological findings of patients with cervical spinal disorders.
References
Fukushima T, Ikata T, Taoka Y & Takata S . Magnetic resonance imaging study on spinal cord plasticity in patients with cervical compression myelopathy. Spine 1991; 16: S534–S538.
Fujiwara K et al. The prognosis of surgery for cervical compression myelopathy. An analysis of the factors involved. J Bone Joint Surg 1989; 71: 393–398.
Koyanagi T et al. Predictability of operative results of cervical spinal compression myelopathy based on preoperative computed tomographic myelography. Spine 1993; 18: 1958–1963.
Matsumoto M et al. Increased signal intensity of the spinal cord on magnetic resonance images in cervical compressive myelopathy. Does it predict the outcome of conservative treatment? Spine 2000; 25: 677–682.
Matsumoto M et al. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg 1998; 80: 19–24.
Sherman JL, Nassaux PY & Citrin CM . Measurements of the normal cervical spinal cord on MR imaging. AJNR 1990; 11: 369–372.
Okada Y, Ikata T, Katoh S & Yamada H . Morphologic analysis of the cervical spinal cord, dural tube, and spinal canal by magnetic resonance imaging in normal adults and patients with cervical spondylotic myelopathy. Spine 1994; 19: 2331–2335.
Holsehelmer J, den Boer JA, Struljk JJ & Rozeboom AR . MR assessment of the normal position of the spinal cord in the spinal canal. AJNR 1994; 15: 951–959.
Suzuki M & Shimamura T . Morphological study of the axial view of the cervical spinal cord by MR images. J Jpn Orthop Assoc 1994; 68: 1–13. (in Japanese).
Tanaka Y . Morphological changes of the cervical spinal canal and cord due to aging. J Jpn Orthop Assoc 1984; 58: 873–886. (in Japanese).
Tanida Y . Morphometrical study of the axial view of the cervical spinal cord with MRI – Analysis of the normal shape and relation between the shape of the spinal cord and the clinical result in compression myelopathy. Central Jpn J Orthop Surg and Traumatol 1996; 39: 1–9. (in Japanese).
Miyasaka K . MR imaging of the spinal cord – with special emphasis on the factors influencing spinal cord measurement. Brain and Nerve 1992; 44: 241–247. (in Japanese).
Czervionke LF, Czervionke JM, Daniels DL & Haughton VM . Characteristic features of MR truncation artifacts. AJNR 1988; 9: 815–824.
Carvlin MJ et al. High-resolution MR of the spinal cord in humans and rats. AJNR 1989; 10: 13–17.
Curtin AJ et al. MR imaging artifacts of the axial internal anatomy of the cervical spinal cord. AJNR 1989; 10: 19–26.
Wolf BS, Khilnani M & Malis L . The sagittal diameter of the bony cervical spinal canal and its significance in cervical spondylosis. J Mt Sinai Hosp 1956; 23: 283–292.
Hinck VC, Gordy PD & Storino HE . Developmental stenosis of the cervical spinal canal. Radiological considerations. Neurology 1964; 14: 864–868.
Hinck VC & Sachdev NS . Developmental stenosis of the cervical spinal canal. Brain 1966; 89: 27–36.
Jones RAC & Thomson JLG . The narrow lumbar canal. J Bone Joint Surg 1968; 50: 595
Acknowledgements
Grant support: Funded by The Marine and Fire Insurance Association of Japan
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ishikawa, M., Matsumoto, M., Fujimura, Y. et al. Changes of cervical spinal cord and cervical spinal canal with age in asymptomatic subjects. Spinal Cord 41, 159–163 (2003). https://doi.org/10.1038/sj.sc.3101375
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101375
Keywords
This article is cited by
-
Congenital Cervical Stenosis: a Review of the Current Literature
Current Reviews in Musculoskeletal Medicine (2023)
-
Extent and characteristic of relationships in canal dimension and canal body ratio between cervical and lumbar spine
Scientific Reports (2021)
-
A comparative shape analysis of the cervical spine between individuals with cervicogenic headaches and asymptomatic controls
Scientific Reports (2021)
-
Magnetic resonance imaging and dynamic X-ray’s correlations with dynamic electrophysiological findings in cervical spondylotic myelopathy: a retrospective cohort study
BMC Neurology (2020)
-
Different patterns of longitudinal brain and spinal cord changes and their associations with disability progression in NMO and MS
European Radiology (2018)