Abstract
Brugada syndrome (BrS) is one of the ion channelopathies associated with sudden cardiac death (SCD). The most common BrS-associated gene (SCN5A) only accounts for approximately 20–25% of BrS patients. This study aims to identify novel mutations across human ion channels in non-familial BrS patients without SCN5A variants through disease-targeted sequencing. We performed disease-targeted multi-gene sequencing across 133 human ion channel genes and 12 reported BrS-associated genes in 15 unrelated, non-familial BrS patients without SCN5A variants. Candidate variants were validated by mass spectrometry and Sanger sequencing. Five de novo mutations were identified in four genes (SCNN1A, KCNJ16, KCNB2, and KCNT1) in three BrS patients (20%). Two of the three patients presented SCD and one had syncope. Interestingly, the two patients presented with SCD had compound mutations (SCNN1A:Arg350Gln and KCNB2:Glu522Lys; SCNN1A:Arg597* and KCNJ16:Ser261Gly). Importantly, two SCNN1A mutations were identified from different families. The KCNT1:Arg1106Gln mutation was identified in a patient with syncope. Bioinformatics algorithms predicted severe functional interruptions in these four mutation loci, suggesting their pivotal roles in BrS. This study identified four novel BrS-associated genes and indicated the effectiveness of this disease-targeted sequencing across ion channel genes for non-familial BrS patients without SCN5A variants.
Similar content being viewed by others
Introduction
In Western countries, sudden cardiac death (SCD) is one of leading causes of mortality, with an incidence of approximately 1 per 1,000 individuals per year1. Five to ten percent of SCD cases are related to rare inherited cardiac arrhythmias, which are typically characterized with a distinctive electrocardiogram (ECG) pattern in the absence of identifiable structural heart disease2. One such disorder is Brugada syndrome (BrS), characterized by ST-segment elevation in right precordial ECG leads3. BrS is a rare life-threatening cardiac arrhythmic disease in adults. The prevalence is approximately 5 per 10,000 in Western countries and higher (12 per 10,000) in Southeast Asia4,5. The average age at the time of initial diagnosis or sudden death is 40 ± 22 years6.
BrS is one of the ion channelopathies associated with dysfunction of sodium, potassium or calcium channels5,7,8. After two decades, SCN5A that encodes sodium channel has emerged as the most common gene associated with BrS and 11 BrS-associated genes was identified thereafter8,9,10,11. However, the disease-causal genes in approximately 60–70% of patients with BrS still remain unclear following studies adopting traditional candidate gene approaches using Sanger sequencing. In other words, the traditional candidate gene approach only resolves less than 30–40% of BrS cases12.
BrS has a genetic basis and the associated model of inheritance is either autosomal dominant with incomplete penetrance or spontaneous mutations. Although some BrS-associated genes were successfully identified through linkage analyses in familial BrS patients, more than 70% of BrS patients have no family history of sudden cardiac death (SCD) or BrS13. Approximately 80% of mutations linked to BrS were sporadic, according to the largest BrS registry (FINGER) in the world14. It would be not feasible to perform a co-segregation analysis in patients with non-familial BrS. However, these patients represent the majority of BrS cases.
Sanger sequencing is a standard technique employed in molecular diagnostics and has been chosen as the main clinical testing method for disorders that are predominantly induced by a single causative gene. However, this traditional genetic screening method is laborious. The development of alternative approaches involving ‘next-generation’ sequencing (NGS) offers a potential solution. In addition, this approach has the capability to investigate the influence of unique and distinct variations in rare polygenetic hereditary diseases, such as retinitis pigmentosa15 or muscular dystrophy16, which can be assayed only through sequencing17.
Since BrS is one of the ion channelopathies, we hypothesized that the disease-causal genes in the remaining 60–70% of patients with BrS were in other ion channel genes. We aimed to comprehensively examine genes associated with human ion channels (sodium, potassium and calcium at NCBI database)12 in non-familial BrS patients through disease-targeted multiple gene sequencing approach.
Methods
Study Subjects
From 2000 to 2010, we recruited symptomatic BrS patients (probands) from medical centers or hospitals in Taiwan (Cohort Of Brugada syndrome in an Asian Chinese Population, COBRA_ChiP). The study protocol was in accordance with the Declaration of Helsinki and was approved by the local ethical committee of National Taiwan University Hospital. All study subjects signed informed consent before participation. BrS was definitively diagnosed by two independent cardiologists based on established criteria (Figure S1)18. Currently, Heart Rhythm Society/European Heart Rhythm Association Expert Consensus Statement recommended to perform genetic testing of SCN5A for patients with a clinical diagnosis of BrS19. Thus, we screened SCN5A mutations for probands first. SCN5A mutations were defined as a case-only variant with amino acid change, i.e., no such mutations were observed in the 500 healthy volunteers (in house control) or public databases20. Since some studies reported that SCN5A SNPs may have a functional impact on BrS21,22, we only included 15 non-familial BrS patients without SCN5A variants for further NGS study.
Exon Capture and Disease-targeted Multi-gene Sequencing
Because BrS is one of the ion channelopathies, we comprehensively examined genes associated with human ion channels (sodium, potassium and calcium at NCBI database)12 through disease-targeted multiple gene sequencing approach. All 12 reported BrS-associated genes12 and 133 genes related to human sodium, calcium and potassium channels (Table S1) were selected for exome in-depth sequencing. All experimental procedures of the exon capture and NGS followed the instructions provided by the manufacturers (supplementary materials). Figure S2 illustrates an overview of the experimental design employed in this study. To maintain the quality of sequencing data, only those reads with a Phred score higher than 20 were analyzed. Bowtie software23 was used to map the sequencing pairs using the database of reference sequences (Refseq) messenger RNA (mRNA) transcripts in human genome version 19. To incorporate mutation information, the maximum number of mismatched alignments was set as three. In other words, in 180 bp of DNA sequences within one sequencing pair, only three loci (1.67%) were allowed to differ from the reference genome. Since the exon capture assay was performed to enrich the DNA of target genes, only those sequencing pairs mapped to the 145 selected genes remained. The average coverage of each sample was approximately 60 (Table S2) and thus 30 was used as the cutoff to call a mutation. Consequently, the following three criteria must be met to be identified as possible mutations: (1) at least 30 reads; (2) result in an amino acid change; (3) not to be reported in the database of SNP (dbSNP) version 135.
Validation by Mass Spectrometry
To validate the potential mutations, two popular commercial mass spectrometry systems, including Illumina VeraCode system (San Diego, CA) and Sequenom system (Sequenom; San Diego, CA), were utilized. All experimental procedures followed the standard protocols (supplementary materials).
Validation by Sanger Sequencing
In addition to validation by mass spectrometry, Sanger sequencing was performed to confirm the mutations. In addition to the BrS patients, DNA from 611 healthy controls (Chinese Han population) was analyzed using the same amplicons. The details of primers and PCR conditions are shown in Tables S3 and S4.
Functional Prediction and Protein-protein Interactions of Identified Mutations
Four bioinformatics algorithms were used to assess the potential functional impacts, including Sorting Intolerant From Tolerant (SIFT)23, Protein Variation Effect Analyzer (Provean)24, Polymorphism Phenotyping-2 (PolyPhen-2)25. Conservation of the mutation loci across different vertebrate species was evaluated by using the UCSC genome browser and the Phylop algorithm26. The protein-protein interactions (PPIs) of the mutations were characterized by using the String database27.
Results
Demographic Characteristics of Studied Non-familial BrS Patients
The average age of the 15 non-familial BrS patients without SCN5A variants at diagnosis was 40 ± 9 years and all were male. Six patients (40%) were resuscitated from SCD and 9 (60%) presented with syncope. Twelve patients (80%) had spontaneous cove-type Brugada ECGs. Ten (67%) received an implantable cardioverter-defibrillator (ICD) implantation. The clinical profile of non-familial BrS patients is presented in Table 1.
Identification of Possible Mutations by Disease-targeted Multi-gene Sequencing
After appropriate quality controls (Phred score ≥ 20), the average number of the remaining sequencing pairs was approximately 2,420,000. The numbers of sequencing pairs in different samples were similar (Table S2), suggesting the stability and consistency of the NGS data. A total of 619 nucleotide alterations were reported in at least one sample and 91 of them had non-synonymous alterations. After excluding 35 alterations reported in dbSNP, the remaining 56 non-synonymous alterations were selected for further investigations.
Validation of Putative Mutations Using Mass Spectrometry
Among the 56 putative mutation loci identified by NGS, 11 variants were successfully confirmed in 8 BrS patients (Table S5). The newly released 1000 Genomes database was used to exclude SNP loci28. Collectively, five de novo mutations in four genes (SCNN1A, KCNJ16, KCNB2, and KCNT1) were identified in 3 BrS patients. Five patients had non-synonymous SNPs and 7 patients showed no mutations or non-synonymous SNPs in these ion channel-associated genes. Lastly, no mutations in previously published BrS-associated genes (BrS2–12) were identified in our BrS patients.
Validation of Five de novo Mutations Using Sanger Sequencing
The results of Sanger sequencing confirmed the five potential mutations were indeed heterozygous mutations in all affected individuals (Figure S3). Table 2 showed the clinical characteristics of the three BrS patients with de novo mutations. Two of them presented SCD and one had syncope; however, none of them had a family history of BrS or SCD. Interestingly, both of the patients presenting SCD had compound mutations (SCNN1A:Arg350Gln and KCNB2:Glu522Lys; SCNN1A:Arg597* and KCNJ16:Ser261Gly). Notably, two SCNN1A mutations (Arg350Gln and Arg597*) were identified from different families, suggesting SCNN1A may play a pivotal role in BrS. Intriguingly, we identified one novel mutation (KCNB2:Arg460Gly) in one of another 22 independent BrS patients (BrS33). This patient (BrS33) presented with SCD and received successfully resuscitation and both of them experienced SCD. Therefore, the results suggested that two KCNB2 mutations (Glu522Lys and Arg460Gly) deserved further investigations since they were identified from different BrS families. Furthermore, we tested DNA samples from the parents of the affected individuals, which showed all mutations occurred de novo. Figure 1 illustrated the relationship between phenotype (ECG) and genotype in these three BrS patients and their family members. All family members were asymptomatic and had no cove-type Brugada ECG. In addition, all family members had normal genotypes of the identified genes, confirming these five mutations were sporadic.
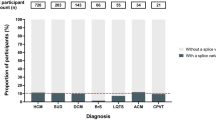
Phenotype and genotype relationship of the five identified mutations in three BrS families, including A. BrS4, B. BrS15 and C. BrS3.
Family pedigrees of the BrS patients with de novo mutations and family members are shown in the upper left panel. Typical Brugada-type ECG and normal ECG in lead V1-V3 is illustrated in the lower left panel. The results of Sanger sequencing in the corresponding patients and their family members, including parents, siblings and children, are summarized in the right panel.
Phylogenetic Analysis and Functional Prediction
We examined whether the five loci were conserved across different species. The amino acid sequences generated from the corresponding mRNA transcripts of 46 species were retrieved from the UCSC genome browser. The Phylop conservation scores in vertebrates were calculated to measure the non-neutral substitution rates of the variants26. The results are illustrated in Figure 2. High conservation percentages (88.9% and 78.9%) and significant Phylop scores (P = 0.0068 and P = 0.0223) were observed in KCNJ16:Ser261Gly and SCNN1A:Arg350Gln. In addition, 36 species (81.8%) showed the wild type sequence in KCNT1:Arg1106Gln, which displayed a markedly significant Phylop score (P = 0.0034). Although the Phylop score of KCNB2:Glu522Lys showed borderline significance, the conservation percentage was still around 80%. SCNN1A:Arg597*, which was relatively less conserved, is a radical mutation (stop codon) causing a truncated protein. Therefore, the results suggested the five highly conserved mutations in these loci might be detrimental.
To assess the potential functional impacts, we utilized genomic evolutionary rate profiling (GERP) score29 and three bioinformatics algorithms, including SIFT23, Provean24 and PolyPhen-225. Intriguingly, GERP scores were significant in all five variants (P < 0.05), suggesting the probability of a substitution of nucleotides in the corresponding locus is low (Table 3). In addition, all three algorithms indicated the deleterious impact of KCNJ16:Ser261Gly and SCNN1A:Arg350Gln (Table 3). Notably, only Provean was capable of predicting the functional influence of an early termination of amino acids, which indicated SCNN1A:Arg597* as deleterious. For KCNT1:Arg1106Gln, SIFT and PolyPhen-2 reported a harmful substitution. SIFT and Provean predicted KCNB2:Glu522Lys as a tolerant change, suggesting this locus may have a lower chance of influencing the pathogenesis of BrS.
Protein-Protein Interactions of Identified de novo Mutations
The String database27 was utilized to analyze potential PPIs of the identified mutations, which contains both known and predicted protein interactions. We focused on two BrS patients (BrS4 and BrS15) because they presented with SCD and had compound mutations (SCNN1A:Arg597* and KCNJ16:Ser261Gly in BrS4; SCNN1A:Arg350Gln and KCNB2:Glu522Lys in BrS15). In the SCNN1A-KCNJ16 pair, both proteins may interact through CFTR and AQP4 (Figure S4A). CFTR is a major chloride channel protein and AQP4 serves as a water-selective channel protein in many cells. They can interact with SCN5A through the proteins related to BrS (Figure S4A). Therefore, their deregulation may lead to an imbalance of membrane potential, which is associated with increased arrhythmogenesis. In the SCNN1A-KCNB2 pair, these two proteins may interact through UBC/KCNH2 and/or NEDD4/KCNQ1 (Figure S4B). One of the major functions of UBC is to control protein degradation. KCNQ1, KCNH2 and KCNH5 belong to the EAG family of voltage-gated potassium channels30. Interestingly, previous studies have demonstrated that mutations or SNPs of KCNQ1 and KCNH2 can cause life-threatening arrhythmia31,32.
Since SCN5A is the most common BrS-associated gene, we also analyzed the interactions between SCN5A and the identified genes. All three of the novel gene-encoded proteins interacted with SCN5A through 1–3 communicators (Figure S4). Therefore, these two pairs of mutations may interact through other channel proteins and deregulations of them may destabilize the membrane potential and thus facilitate their abnormal function.
Discussion
In this study, we not only identified 4 de novo BrS-associated genes but also demonstrated a new approach to sequencing disease-targeted multiple ion channel genes, which may increase the mutation yield in non-familial SCN5A-negative BrS patients. This approach could be used as an effective genetic screening method for SCN5A-negative BrS patients in the future.
In 2011, the Heart Rhythm Society/European Heart Rhythm Association Expert Consensus Statement recommended to perform genetic testing of SCN5A only for patients with a clinical diagnosis of BrS19. However, SCN5A (BrS1) only accounts for approximately 25% of BrS in Caucasian populations4, even lower proportion in the Chinese Han population (7.5–8%)20. In addition to sodium channel dysfunction, mutations involving calcium channels encoded by CACNA1C, CACNB2B, and CACNA2D1 may cause BrS cases. Mutations of genes encoding potassium current (KCNE3 and KCND3) or the IkATP current (KCNJ8) were also identified in the past years8,9,10,11. Over the past 20 years, 11 BrS-associated genes (BrS2 through BrS12) were identified. However, the mutation rate of them was still relatively low. In 2012, for example, Crotti et al. reported that only 5% of the mutation yield was identified in newly identified 11 BrS-associated genes (BrS2-12). On the other hand, more than 70% of BrS patients have no family history of BrS or SCD13. Therefore, it is hard to perform co-segregation analyses in these non-familial patients. Considering current genetic findings and underlying pathogenic electrophysiology of BrS, we employed a new approach to sequence disease-targeted multiple genes on human ion channel genes in non-familial BrS patients. This study successfully identified four de novo genes in three of the fifteen (20%) non-familial BrS patients who were detected to be without SCN5A variants using Sanger sequencing.
Interestingly, two of the three BrS patients presenting with SCD were found to have compound mutations (SCNN1A:Arg350Gln and KCNB2:Glu522Lys; SCNN1A:Arg597* and KCNJ16:Ser261Gly). Importantly, SCNN1A:Arg350Gln and SCNN1A:Arg597* two were identified from not only different genomic positions in the same gene but also from different families. These results further strengthened that these two mutations are causative. In addition, SCNN1A:Arg597* is a radical mutation (stop codon) and is predicted as deleterious substitution by Provean. Moreover, all three algorithms indicated KCNJ16:Ser261Gly and SCNN1A:Arg350Gln as possibly harmful variants. These two mutations showed 89% and 79% conservation in 46 species, suggesting they were not mutation hotspots. Thus, the corresponding nucleotide changes have high potential of influencing the pathogenesis of BrS.
The four newly identified de novo genes were reported to be expressed in human heart tissues33,34,35. However, the association between these genes and arrhythmia has not been investigated previously. SCNN1A encodes the alpha subunit of amiloride-sensitive sodium channels, which control fluid and electrolyte transportation. Mutations of this gene have been associated with sodium imbalance that may predispose the heart to life-threatening arrhythmia36. KCNJ16 (hKir5.1) is located at chromosome 17q23.1-24.2 and is separated by 34 kb from KCNJ2 (hKir2.1). When expressed in Xenopus oocytes, Kir5.1 is able to target the cell surface efficiently and form electrically silent channels together with Kir2.1. The interaction between them can inhibit the activity of the Kir2.1 channel in native cells, which has been associated with cardiac arrhythmia37. KCNB2 encodes a voltage-gated delayed rectifier potassium channel and was reported to contribute to the resting membrane potential in myocytes38. Mutated KCNB2 may result in arrhythmia due to unsteady resting membrane potential. KCNT1 encodes the sodium-activated potassium channel subunit (KCa4.1) and is similar in sequence to a calcium-activated potassium channel (SLACK)33,39,40. The intracellular C terminus of KCNT1 is regulated by protein kinase C via multiple phosphorylation sites. The p.Arg1106Gln alternation observed in BrS3 patients occurs within the C-terminal region of KCNT1, which is immediately adjacent to a nicotinamide adenine dinucleotide (NAD+)-binding site involved in the modulation of the channel33. Notably, the affected individuals with these mutations were identified with SCD, syncope, or seizure and showed spontaneous coved-type Brugada ECGs; all received resuscitation successfully.
There are certain limitations to our study. First, we performed disease-targeted multiple gene sequencing instead of whole exome sequencing. This may miss some possible BrS-associated mutations. However, the mutation rates in other non-ion channel associated genes are more likely to be very low because all BrS patients have abnormal 12-lead ECG clinically and most subtypes of BrS are essentially a disease involving ion channel dysfunction. Second, we did not perform in vitro or in vivo functional studies to demonstrate the pathological impacts of these newly identified genes on BrS. However, all identified de novo mutations are highly conserved in their amino acid residues and were neither detected in their ancestry-matched controls nor present in the variant databases. A previous study has also shown that utilizing multiple in silico analyses can facilitate identification of novel variants in BrS41. Because all mutations were predicted to be pathogenic or possibly pathogenic and are known to be expressed in human heart tissues33,34,35, these genes appear to be involved in the development of cardiac arrhythmia. Third, the NGS method is not capable of reliably identifying the structural variations associated with disease. This might have contributed to the identification of some BrS patients without ion channel-associated genetic mutations in this study.
References
Straus, S. M. et al. The incidence of sudden cardiac death in the general population. J Clin Epidemiol 57, 98–102 (2004).
Priori, S. G. et al. Task Force on Sudden Cardiac Death, European Society of Cardiology. Europace 4, 3–18 (2002).
Brugada, P. & Brugada, J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol 20, 1391–6 (1992).
Mizusawa, Y. & Wilde, A. A. Brugada syndrome. Circ Arrhythm Electrophysiol 5, 606–16 (2012).
Berne, P. & Brugada, J. Brugada syndrome 2012. Circ J 76, 1563–71 (2012).
Juang, J. M. et al. Characteristics of Chinese patients with symptomatic Brugada syndrome in Taiwan. Cardiology 99, 182–9 (2003).
Hedley, P. L. et al. The genetic basis of Brugada syndrome: a mutation update. Hum Mutat 30, 1256–66 (2009).
Antzelevitch, C. et al. Loss-of-function mutations in the cardiac calcium channel underlie a new clinical entity characterized by ST-segment elevation, short QT intervals and sudden cardiac death. Circulation 115, 442–9 (2007).
Burashnikov, E. et al. Mutations in the cardiac L-type calcium channel associated with inherited J-wave syndromes and sudden cardiac death. Heart Rhythm 7, 1872–82 (2010).
Giudicessi, J. R. et al. Transient outward current (I(to)) gain-of-function mutations in the KCND3-encoded Kv4.3 potassium channel and Brugada syndrome. Heart Rhythm 8, 1024–32 (2011).
Medeiros-Domingo, A. et al. Gain-of-function mutation S422L in the KCNJ8-encoded cardiac K(ATP) channel Kir6.1 as a pathogenic substrate for J-wave syndromes. Heart Rhythm 7, 1466–71 (2010).
Crotti, L. et al. Spectrum and prevalence of mutations involving BrS1- through BrS12-susceptibility genes in a cohort of unrelated patients referred for Brugada syndrome genetic testing: implications for genetic testing. J Am Coll Cardiol 60, 1410–8 (2012).
Probst, V. et al. Long-term prognosis of patients diagnosed with Brugada syndrome: Results from the FINGER Brugada Syndrome Registry. Circulation 121, 635–43 (2010).
Veerakul, G. & Nademanee, K. Brugada syndrome: two decades of progress. Circ J 76, 2713–22 (2012).
O'Sullivan, J. et al. A paradigm shift in the delivery of services for diagnosis of inherited retinal disease. J Med Genet 49, 322–6 (2012).
Valencia, C. A. et al. Comprehensive mutation analysis for congenital muscular dystrophy: a clinical PCR-based enrichment and next-generation sequencing panel. PLoS One 8, e53083 (2013).
Rehm, H. L. Disease-targeted sequencing: a cornerstone in the clinic. Nat Rev Genet 14, 295–300 (2013).
Antzelevitch, C. et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation 111, 659–70 (2005).
Ackerman, M. J. et al. HRS/EHRA expert consensus statement on the state of genetic testing for the channelopathies and cardiomyopathies: this document was developed as a partnership between the Heart Rhythm Society (HRS) and the European Heart Rhythm Association (EHRA). Europace 13, 1077–109 (2011).
Juang, J.-M. J. et al. Unique clinical characteristics and SCN5A mutations in patients with Brugada syndrome in Taiwan. JFMA, 10.1016/j.jfma.2013.02.002 (2013) [In press].
Tan, B. H. et al. Common human SCN5A polymorphisms have altered electrophysiology when expressed in Q1077 splice variants. Heart Rhythm 2, 741–7 (2005).
Poelzing, S. et al. SCN5A polymorphism restores trafficking of a Brugada syndrome mutation on a separate gene. Circulation 114, 368–76 (2006).
Kumar, P., Henikoff, S. & Ng, P. C. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc 4, 1073–81 (2009).
Choi, Y., Sims, G. E., Murphy, S., Miller, J. R. & Chan, A. P. Predicting the functional effect of amino acid substitutions and indels. PLoS One 7, e46688 (2012).
Adzhubei, I. A. et al. A method and server for predicting damaging missense mutations. Nat Methods 7, 248–9 (2010).
Pollard, K. S., Hubisz, M. J., Rosenbloom, K. R. & Siepel, A. Detection of nonneutral substitution rates on mammalian phylogenies. Genome Res 20, 110–21 (2010).
Szklarczyk, D. et al. The STRING database in 2011: functional interaction networks of proteins, globally integrated and scored. Nucleic Acids Res 39, D561–8 (2011).
Abecasis, G. R. et al. An integrated map of genetic variation from 1,092 human genomes. Nature 491, 56–65 (2012).
Cooper, G. M. et al. Distribution and intensity of constraint in mammalian genomic sequence. Genome Res 15, 901–13 (2005).
Rebhan, M., Chalifa-Caspi, V., Prilusky, J. & Lancet, D. GeneCards: integrating information about genes, proteins and diseases. Trends Genet 13, 163 (1997).
Wilders, R. & Verkerk, A. O. Role of the R1135H KCNH2 mutation in Brugada syndrome. Int J Cardiol 144, 149–51 (2010).
Kubota, T. et al. Evidence for a single nucleotide polymorphism in the KCNQ1 potassium channel that underlies susceptibility to life-threatening arrhythmias. J Cardiovasc Electrophysiol 12, 1223–9 (2001).
Heron, S. E. et al. Missense mutations in the sodium-gated potassium channel gene KCNT1 cause severe autosomal dominant nocturnal frontal lobe epilepsy. Nat Genet 44, 1188–90 (2012).
Harrell, M. D., Harbi, S., Hoffman, J. F., Zavadil, J. & Coetzee, W. A. Large-scale analysis of ion channel gene expression in the mouse heart during perinatal development. Physiol Genomics 28, 273–83 (2007).
Sato, A. et al. Cerebellar development transcriptome database (CDT-DB): profiling of spatio-temporal gene expression during the postnatal development of mouse cerebellum. Neural Netw 21, 1056–69 (2008).
Riepe, F. G. Clinical and molecular features of type 1 pseudohypoaldosteronism. Horm Res 72, 1–9 (2009).
Derst, C. et al. Genetic and functional linkage of Kir5.1 and Kir2.1 channel subunits. FEBS Lett 491, 305–11 (2001).
Malysz, J. et al. The Kv2.2 alpha subunit contributes to delayed rectifier K(+) currents in myocytes from rabbit corpus cavernosum. J Androl 23, 899–910 (2002).
Bhattacharjee, A., Gan, L. & Kaczmarek, L. K. Localization of the Slack potassium channel in the rat central nervous system. J Comp Neurol 454, 241–54 (2002).
Bhattacharjee, A., von Hehn, C. A., Mei, X. & Kaczmarek, L. K. Localization of the Na+-activated K+ channel Slick in the rat central nervous system. J Comp Neurol 484, 80–92 (2005).
Juang, J. M. et al. Utilizing multiple in silico analyses to identify putative causal SCN5A variants in Brugada syndrome. Sci Rep 4, 3850, 10.1038/srep03850 (2014).
Acknowledgements
We are sincerely grateful to many cardiologists, including Dr. Shih-Ann Chen, Dr. Tsu-Juey Wu, Dr. Shoei K. Stephen Huang, Dr. Yenn-Jiang Lin, Dr. Chun-Chieh Wang, Dr. Chi-Tai Kuo, Dr. Yu-Feng Hu, Dr. Kwo-Chang Ueng, Dr. Hsuan-Ming Tsao, Dr. Kuan-Cheng Chang, Dr. Meng-Huan Lei, Dr. An-Ning Feng, Dr. Chi-Woon Kong, Dr. Wen-Chin Ko, Dr. Jin-Long Huang, Dr. Wen-Chin Tsai, Dr. Chin-Feng Tsai, Dr. Li-Wei Lo, Dr. Huey-Ming Lo, Dr. Meng-Cheng Chiang, Dr. Chih-Ping Hsia, Dr. Jen-Fu Liu, Dr. Shuenn-Nan Chiu, Dr. Mei-Hwan Wu, Dr. Ming-Tai Lin, Dr. Su-Kiat Chua and many other doctors in other medical centers or hospitals for referring patients to our hospital and to the staff of the Sixth Core Lab, Department of Medical Research, National Taiwan University Hospital for technical support. We also thank the technical/bioinformatics services provided by the National Center for Genome Medicine of the National Core Facility Program for Biotechnology, National Science Council. The authors declare no potential conflicts of interest. Financial support for this research was provided partially through grants NTUH 98-N1266, NTUH100-N1775, VN100-08, NTUH101-N2010, NTUH101-S1780, VN101-04, NTUH 101-S1784, NTUH 102-M2224, NTUH.102-S2099, NTUH 102-S2035, NTUH 103-S2326, NTUH 103-L004, UN102-019 and UN 103-018 from National Taiwan University Hospital, YongLin Biomedical Center, National Taiwan University and NSC 101-2314-B-002-168-MY2, NSC 101-2314-B-002-173-MY2, NSC 103-2314-B-002-148 from Ministry of Science and Technology.
Author information
Authors and Affiliations
Contributions
J.M.J.J., T.P.L., E.Y.C., L.P.L. and J.L.L. conceived and designed the experiments. J.M.J.J. and S.F.S.Y. performed the experiments. J.M.J.J., T.P.L. and C.C.H. analyzed the data. J.M.J.J., Y.B.L., C.T.T., L.Y.L., C.C.Y., W.J.C., F.T.C., E.Y.C., L.P.L. and J.L.L. contributed reagents, materials, and/or analysis tools. J.M.J.J., T.P.L., L.C.L. and E.Y.C. wrote the paper.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Supplementary Information
Supplementary data
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Juang, JM., Lu, TP., Lai, LC. et al. Disease-Targeted Sequencing of Ion Channel Genes identifies de novo mutations in Patients with Non-Familial Brugada Syndrome. Sci Rep 4, 6733 (2014). https://doi.org/10.1038/srep06733
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep06733
This article is cited by
-
Gene mutations in comorbidity of epilepsy and arrhythmia
Journal of Neurology (2023)
-
Interaction Between HCN and Slack Channels Regulates mPFC Pyramidal Cell Excitability in Working Memory Circuits
Molecular Neurobiology (2023)
-
Epilepsy and brain channelopathies from infancy to adulthood
Neurological Sciences (2020)
-
Early Treatment with Quinidine in 2 Patients with Epilepsy of Infancy with Migrating Focal Seizures (EIMFS) Due to Gain-of-Function KCNT1 Mutations: Functional Studies, Clinical Responses, and Critical Issues for Personalized Therapy
Neurotherapeutics (2018)
-
ADAM9 promotes lung cancer progression through vascular remodeling by VEGFA, ANGPT2, and PLAT
Scientific Reports (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.