Summary
Synopsis
Fosfomycin tromethamine is a phosphonic acid bactericidal agent with in vitro activity against most urinary tract pathogens. It is particularly active against Escherichia coli, and Citrobacter, Enterobacter, Klebsiella, Serratia and Enterococcus spp. There appears to be little cross-resistance between fosfomycin and other antibacterial agents, possibly because it differs from other agents in its general chemical structure and site of action.
In its new formulation as the oral tromethamine salt, fosfomycin has 34 to 41% oral bioavailability, has a mean elimination half-life of 5.7 hours, and is primarily excreted unchanged in the urine. Following a single 3g oral dose, peak urinary concentrations occur within 4 hours and remain high (>128 mg/L) for 24 to 48 hours, which is sufficient to inhibit most urinary tract pathogens.
In clinical trials in patients with acute uncomplicated lower urinary tract infection, single-dose fosfomycin tromethamine therapy was effective, and comparable with several other antibacterial agents given either as single-dose or multiple-dose treatments [e.g. β-lactam and fluoroquinolone agents, cotrimoxazole (trimethoprim-sulfamethoxazole), nitrofurantoin and pipemidic acid]. Bacteriological eradication rates of 75 to 90% were achieved 5 to 11 days after therapy, with eradication rates of 62 to 93% 4 to 6 weeks after therapy. In 3 large double-blind comparisons with ciprofloxacin, cotrimoxazole and nitrofurantoin, 99% of fosfomycin tromethamine recipients and 100% of patients receiving comparator agents were considered clinically cured or improved after therapy.
Fosfomycin tromethamine is well tolerated, with a low incidence of adverse events. These comprise mainly gastrointestinal symptoms that are transient, mild and self-limiting.
Thus, fosfomycin tromethamine achieves high clinical and bacteriological cure rates in patients with acute uncomplicated lower urinary tract infection and is well tolerated. The single-dose administration regimen and favourable US pregnancy category rating of fosfomycin tromethamine should also encourage its use in this indication.
Antibacterial Activity
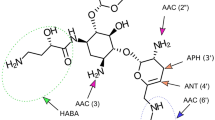
Fosfomycin tromethamine is a bactericidal phosphonic acid derivative which acts primarily by inhibiting bacterial cell wall (peptidoglycan) synthesis. It has antibacterial activity against many pathogenic and opportunistic Gram-positive and Gram-negative bacteria isolated from patients with lower urinary tract infections (UTI). According to conventional in vitro susceptibility tests, fosfomycin has good activity against Escherichia coli, Staphylococcus aureus, and Serratia, Klebsiella, Citrobacter, Enterococcus and Enterobacter spp. Minimum inhibitory concentrations active against 90% of isolates (MIC90 values) for some other important pathogens are relatively high, but are well within the urinary concentrations of fosfomycin achieved during treatment with the drug.
In vitro studies modelling bladder fill and voiding (to simulate fluctuations of fosfomycin concentrations) indicate that sufficiently high concentrations of fosfomycin are achieved after a single 3g dose to attain >99% kill rates against common urinary pathogens. Bacterial adhesiveness to uroepithelial mucosa is reduced within 1 hour after exposure to fosfomycin 1000 mg/L.
Bacterial resistance to fosfomycin can be either chromosomal or, more rarely, plasmid-mediated. The frequency of in vitro fosfomycin-resistant mutants is low, and there appears to be little cross-resistance between fosfomycin and other antibacterial agents.
Small changes to the faecal flora of healthy volunteers generally occur 2 to 4 days after administration but usually return to baseline levels within 2 to 3 weeks.
Pharmacokinetic Properties
Following a single oral dose of fosfomycin tromethamine (≡3g fosfomycin), mean peak plasma concentrations (Cmax) range from 22 to 32 mg/L and are reached between 2 and 2.5 hours (tmax). The bioavailability of a single 3g oral dose ranges from 34 to 41%, and from 54 to 65% when expressed as a proportion of the oral dose recovered in the urine.
The mean terminal elimination half-life (t1/2β) of fosfomycin is 5.7 hours. The drug is primarily excreted unchanged in the urine; <0.5% is eliminated by the biliary route. Mean peak urinary concentrations of fosfomycin occur within 4 hours after a single 3g dose, and generally range from 1053 to 4415 mg/L. Approximately 32 to 43% of a single dose is excreted within 48 hours and, of this, approximately 85 to 95% is excreted within 24 hours. Nonetheless, fosfomycin concentrations >128 mg/L, which are sufficient to inhibit most urinary pathogens, are maintained for 24 to 48 hours after a single 3g oral dose.
In patients with renal impairment (creatinine clearance <45 ml/min), the Cmax of fosfomycin is increased, tmax and t1/2β are prolonged and urinary elimination is reduced.
Therapeutic Efficacy
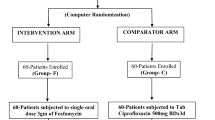
Comparative nonblind and double-blind studies in patients (predominantly women) with acute uncomplicated lower UTI indicate that a single 3g oral dose of fosfomycin tromethamine is as bacteriologically effective as single oral doses of amoxicillin, cotrimoxazole (trimethoprim-sulfamethoxazole), norfloxacin, ofloxacin or pefloxacin. Single-dose fosfomycin tromethamine is also as effective as multiple-dose regimens of amoxicillin-clavulanic acid, cefalexin, nitrofurantoin, norfloxacin, pipemidic acid or shorter (3-day) cotrimoxazole therapy. It was slightly less effective than ciprofloxacin 250mg twice daily for 7 days and a longer (10-day) cotrimoxazole regimen.
In double-blind studies, a single 3g oral dose of fosfomycin tromethamine produced bacteriological cure after 5 to 11 days in 75 to 90% of patients with lower UTI (compared with 76 to 97% of patients receiving comparator agents) and 62 to 93% of patients after 4 to 6 weeks (compared with 65 to 96% of patients receiving comparator agents). Reinfection rates were 8 to 13% in fosfomycin tromethamine recipients and 6 to 16% in control treatment groups. In 3 large double-blind comparisons with ciprofloxacin, cotrimoxazole and nitrofurantoin (237 to 273 evaluable patients per treatment arm), 99% of fosfomycin tromethamine recipients and 100% of patients receiving comparator agents were considered clinically cured or improved after therapy.
Limited data concerning single-dose fosfomycin tromethamine therapy for children and pregnant women with acute uncomplicated lower UTI suggest that it is as well tolerated and as effective as pipemidic acid, nitrofurantoin, or netilmicin.
Tolerability
Single 3g oral doses of fosfomycin tromethamine appear to be well tolerated. Adverse events are transient and tend to resolve spontaneously within 1 to 2 days. Mild, self-limiting gastrointestinal disturbances (predominantly diarrhoea) are the most frequently reported events. Other commonly reported minor adverse events include dizziness and/or headache, and vaginitis.
Fetotoxicity was not detected in a study of 291 pregnant women treated with fosfomycin tromethamine or pipemidic acid. Fosfomycin tromethamine has been rated ‘pregnancy category B’ in the US indicating it may be used in pregnancy if clearly needed.
Dosage and Administration
A single oral dose of fosfomycin tromethamine (equivalent to 3g of fosfomycin) is recommended in the treatment of acute uncomplicated lower UTI in adults. Fosfomycin tromethamine is not generally recommended for children, although in some countries a single oral dose equivalent to fosfomycin 2g is approved for children aged ≥5 years.
Concomitant administration of metoclopramide is not advised, since it has been shown to lower serum and urinary concentrations of fosfomycin tromethamine.
Similar content being viewed by others
References
Hendlin D, Stapley EO, Jackson M, et al. Phosphonomycin, a new antibiotic produced by strains of Streptomyces. Science 1969; 166: 122–3
Kahan FM, Kahan JS, Cassidy PJ, et al. The mechanism of action of fosfomycin (phosphonomycin). Ann NY Acad Sci 1974; 235: 364–86
Minassian MA, Williams JD. The clinical pharmacology of fosfomycin trometamol. Rev Contemp Pharmacother 1995; 6(2): 45–53
Fujii R. Fosfomycin in the treatment of bacterial infections: summary of clinical trials in Japan. Chemotherapy 1977; 23Suppl 1: 234–46
Greenwood D. Fosfomycin trometamol and the single-dose treatment of cystitis. J Med Microbiol 1994; 41: 293–4
Ferrari V, Bonanomi L, Borgia M, et al. A new fosfomycin derivative with much improved bioavailability by oral route. Chemiother Antimicrob 1981; 4: 59–63
Hooton TM. The epidemiology of urinary tract infection and the concept of significant bacteria. Infection 1990; 18Suppl. 2: S40–3
Reeves DS. Fosfomycin trometamol. J Antimicrob Chemother 1994; 34: 853–8
Zinner SH. Pathogenesis of urinary tract infection. A brief overview. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 9–18
Fihn SD, Latham RH, Roberts P, et al. Association between diaphragm use and urinary tract infection. JAMA 1985; 254(2): 240–5
Peddie BA, Gorrie SI, Bailey RR. Diaphragm use and urinary tract infection [letter]. JAMA 1986; 255(13): 1707
Bailey RR. Management of lower urinary tract infections. Drugs 1993; 45Suppl. 3: 139–44
Kunin CM. Urinary tract infections in females. Clin Infect Dis 1994; 18: 1–12
Nicolle LE. The optimal management of lower urinary tract infections. Infection 1990; 18Suppl. 2: S50–2
Schaeffer AJ, Jones JM, Dunn JK. Association of in vitro Escherichia coli adherence to vaginal and buccal epithelial cells with susceptibility of women to recurrent urinary tract infections. N Engl J Med 1981; 304: 1062–6
Johnson JR. Virulence factors in Escherichia coli urinary tract infection. Clin Microbiol Rev 1991; 4(1): 80–128
Sobel JD, Kaye D. Host factors in the pathogenesis of urinary tract infections. Am J Med 1984; 76: 122–30
Barry AL, Fuchs PC. In vitro susceptibility testing procedures for fosfomycin tromethamine. Antimicrob Agents Chemother 1991 Jun; 35: 1235–8
Delia Bella D, Ferrari V. Monuril: historical background. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 116–20
Greenwood D, Jones A, Eley A. Factors influencing the activity of the trometamol salt of fosfomycin. Eur J Clin Microbiol 1986 Feb; 5: 29–34
Pfaller MA, Barry AL, Fuchs PC. Evaluation of disk susceptibility testing of fosfomycin tromethamine. Diagn Microbiol Infect Dis 1993 Jul; 17: 67–70
Wise R, Andrews J. The bacteriology of fosfomycin trometamol and susceptibility testing in a routine laboratory. Rev Contemp Pharmacother 1995; 6(2): 85–91
Buisson Y, Nicand E, Baccarani R, et al. In vitro susceptibility testing to fosfomycin trometamol of bacterial strains isolated in France from urinary tract infections in out-patients [in French]. Med Mal Infect 1992 Oct; 22: 859–64
Reeves DS, Holt HA, Bywater MJ. In vitro study of fosfomycin trometamol. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 224–31
King A, Phillips I. Comparative in vitro activity of fosfomycin trometamol against urinary tract pathogens. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 242–9
Gismondo MR, Romeo MA, Lo Bue AM, et al. Microbiological basis for the use of fosfomycin trometamol as single-dose therapy for simple cystitis. Chemioterapia 1986 Aug; 5: 278–82
Ferrara A, Migliori PD, Piccioni PD, et al. Influence of experimental conditions on in vitro activity of fosfomycin trometamol and emergence of resistant variants. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 269–83
Rossi L, Fontana R, Meloni GA. In vitro testing of the antibacterial activity of fosfomycin trometamol against urinary pathogens. Chemioterapia 1988 Feb; 7: 10–4
Lerner SA, Price S, Kulkarni S. Microbiological studies of fosfomycin trometamol against urinary isolates in vitro. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 121–9
Wise R, Andrews JM. Fosfomycin trometamol: An in vitro study. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 232–41
Hamilton-Miller JMT. In vitro activity of fosfomycin against problem Gram-positive cocci. Microbios 1992; 71(287): 95–103
Barry AL, Brown SD. Antibacterial spectrum of fosfomycin trometamol. J Antimicrob Chemother 1995; 35: 228–30
Greenwood D. Fosfomycin trometamol: activity in vitro against urinary tract pathogens. Infection 1990; 18Suppl. 2: 60–4
Greenwood D, Coyle S, Andrew J. The trometamol salt of fosfomycin: microbiological evaluation. Eur Urol 1987; 13Suppl 1: 69–75
Greenwood D, Brown J, Edwards R. The influence of anaerobiosis on the activity of fosfomycin trometamol. Infection 1992; 20Suppl. 4: S 305–9
Inouye S, Watanabe T, Tsuruoka T, et al. An increase in the antimicrobial activity in vitro of fosfomycin under anaerobic conditions. J Antimicrob Chemother 1989 Nov; 24: 657–66
Borsotto M, Cuffini AM, Savoia D, et al. In vitro and in vivo activity of fosfomycin trometamol towards mutant bacterial strains. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 261–8
Albini E, Arena E, Belluco G, et al. Adhesion of bacteria to human uroepithelial cells and bactericidal activity of fosfomycin trometamol. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 250–4
Cornaglia G, Pompei R, Foddis G, et al. Antibacterial activity of fosfomycin trometamol in an in vitro model of the urinary bladder. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 255–60
Greenwood D. Activity of the trometamol salt of fosfomycin in an in vitro model of the treatment of bacterial cystitis. Infection 1986 Jul–Aug; 14: 186–9
Arca P, Hardisson C, Suarez JE. Purification of a glutathione S-transferase that mediates fosfomycin resistance in bacteria. Antimicrob Agents Chemother 1990 May; 34: 844–8
Tsuruoka T, Yamada Y. Charactertization of spontaneous fosfomycin (phosphonomycin)-resistant cells of Escherichia coli B in vitro. J Antibiot Tokyo 1975 Nov; 28: 906–11
Kadner RJ, Winkler HH. Isolation and characterization of mutations affecting the transport of hexose phosphates in Escherichia coli. J Bacteriol 1973; 113: 895–900
Venkateswaran PS, Wu HC. Isolation and characterisation of a phosphonomycin-resistant mutant of Escherichia coli K-12. J Bacteriol 1972; 110: 935–44
Suarez JE, Mendoza MC. Plasmid-encoded fosfomycin resistance. Antimicrob Agents Chemother 1991 May; 35: 791–5
Arca P, Rico M, Brana AF, et al. Formation of an adduct between fosfomycin and glutathione: a new mechanism of antibiotic resistance in bacteria. Antimicrob Agents Chemother 1988 Oct; 32: 1552–6
Schito GC, Chezzi C, Nicoletti G, et al. Susceptibility of frequent urinary pathogens to fosfomycin trometamol and eight other antibiotics: results of an Italian multicenter survey. Infection 1992; 20Suppl. 4: 291–5
Greenwood D, Edwards R, Brown J, et al. The comparative activity of fosfomycin trometamol against organisms isolated from infected urines. Infection 1992; 20Suppl. 4: 302–4
Babb JR, Davies JG, Ayliffe GAJ. Effect of a single dose of fosfomycin trometamol on the resident skin flora. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 284–91
Reeves DS, Holt HA, Bywater MJ, et al. Effect of fosfomycin trometamol on the faecal flora of eight healthy volunteers. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 292–8
Bergan T, Thorsteinsson SB, Albini E. Pharmacokinetic profile of fosfomycin trometamol. Chemotherapy (Basel) 1993 Sep–Oct; 39: 297–301
Bergan T. Degree of absorption, pharmacokinetics of fosfomycin trometamol and duration of urinary antibacterial activity. Infection 1990; 18Suppl. 2: 65–9
Bergogne-Berezin E, Muller-Serieys C, Joly-Guillou ML, et al. Trometamol-fosfomycin (Monuril) bioavailability and food-drug interaction. Eur Urol 1987; 13Suppl 1: 64–8
Segre G, Bianchi E, Cataldi A, et al. Pharmacokinetic profile of fosfomycin trometamol (Monuril). Eur Urol 1987; 13Suppl 1: 56–63
Bergan T, Mastropaolo G, Di Mario F, et al. Pharmacokinetics of fosfomycin and influence of cimetidine and metoclopramide on the bioavailability of fosfomycin trometamol. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 157–66
Wilson P, Williams JD, Rolandi E. Comparative pharmacokinetics of fosfomycin trometamol, sodium fosfomycin and calcium fosfomycin in humans. In: Neu H, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 136–42
Monurol package insert. Forest Laboratories Inc. USA. 1996
Bergan T. Pharmacokinetics of fosfomycin. Rev Contemp Pharmacother 1995; 6(2): 55–62
Kirby WMM. Pharmacokinetics of fosfomycin. Chemotherapy 1977; 23Suppl 1: 141–51
Kestle DG, Kirby W. Clinical pharmacology and in vitro activity of phosphonomycin. Antimicrob Agents Chemother 1970; 1969: 332–7
Bergan T. Pharmacokinetic comparison between fosfomycin and other phosphonic acid derivatives. Chemotherapy 1990 Nov; 36Suppl. 1: 10–8
Muller-Serieys C, Bergogne-Berezin E, Joly-Guillou ML. Fosfomycin-trometamol (monuril): pharmacokinetics and food-drug interactions [in French]. Pathol Biol Paris 1987 Jun; 35 (5 Pt 2): 753–6
Muller-Serieys C, Bergogne-Berezin E. Pharmacokinetics of fosfomycin trometamol (Monuril) in healthy volunteers. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 299–301
Fillastre JP, Leroy A, Humbert G, et al. Comparative pharmacokinetics of trometamol-fosfomycin versus calcium-fosfomycin in elderly and uraemic patients. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 143–56
Salvioli G. Oral bioavailability of Z 1282 in elderly patients. Data on file. Forest Laboratories, Inc., USA.
Fillastre JP, Leroy A, Josse S, et al. Pharmacokinetics of trometamol-fosfomycin in uraemic patients [in French]. Pathol Biol Paris 1988 Jun; 36 (5 Pt 2): 728–30
Janknegt R, Hooymans PM, Fabius GTJ, et al. Urinary concentrations of fosfomycin after a single 3g dose of fosfomycin to elderly nursing-home patients. Pharm World Sci 1994 Jun 10;16: 149–53
Cooper J, Raeburn A, Brumfitt W, et al. Single dose and conventional treatment for acute bacterial and non-bacterial dysuria and frequency in general practice. Infection 1990 Mar–Apr; 18: 65–9
Cortes R, Pascual T, Lou-Arnal S, et al. Single oral dose of phosphomycin trometamol versus pipemidic acid and norfloxacin in treating uncomplicated low-level urinary tract infections [in Spanish]. Aten Primaria 1992 Dec; 10: 1007–12
Crocchiolo P. Single-dose fosfomycin trometamol versus multiple-dose cotrimoxazole in the treatment of lower urinary tract infections in general practice. Multicenter Group of General Practitioners. Chemotherapy 1990; 36Suppl 1: 37–40
de-Jong Z, Pontonnier F, Plante P. Single-dose fosfomycin trometamol (Monuril) versus multiple-dose norfloxacin: results of a multicenter study in females with uncomplicated lower urinary tract infections. Urol Int 1991; 46: 344–8
Elhanan G, Tabenkin H, Yahalom R, et al. Single-dose fosfomycin trometamol versus 5-day cephalexin regimen for treatment of uncomplicated lower urinary tract infections in women. Antimicrob Agents Chemother 1994 Nov; 38: 2612–4
Ferraro G, Ambrosi G, Bucci L, et al. Fosfomycin trometamol versus norfloxacin in the treatment of uncomplicated lower urinary tract infections of the elderly. Chemotherapy 1990; 36Suppl 1: 46–9
Jardin A. A general practitioner multicenter study: fosfomycin trometamol single dose versus pipemidic acid multiple dose. Infection 1990; 18Suppl. 2: 89–93
Reynaert J, Van-Eyck D, Vandepitte J. Single dose fosfomycin trometamol versus multiple dose norfloxacin over three days for uncomplicated UTI in general practice. Infection 1990; 18Suppl 2: S 77–9
Zinner S. Fosfomycin trometamol versus pipemidic acid in the treatment of bacteriuria in pregnancy. Chemotherapy (Basel) 1990 Nov; 36Suppl. 1: 50–2
Naber KG, Thyroff-Friesinger U. Fosfomycin trometamol versus ofloxacin/co-trimoxazole as single dose therapy of acute uncomplicated urinary tract infection in females: a multicentre study. Infection 1990; 18Suppl. 2: 70–6
Boerema JBJ, Willems FTC. Fosfomycin trometamol in a single dose versus norfloxacin for seven days in the treatment of uncomplicated urinary tract infections in general practice. Infection 1990; 18Suppl. 2: 80–8
Neu HC. Fosfomycin trometamol versus amoxycillin — single-dose multicenter study of urinary tract infections. Chemotherapy (Basel) 1990 Nov; 36Suppl. 1: 19–23
Richaud C. Single dose treatment of lower urinary tract infection in women: results of a trial with fosfomycin trometamol versus pefloxacin. Med Mal Infect 1995; 25: 154–9
Selvaggi FP, Ditonno P, Traficante A, et al. Fosfomycin trometamol (Monuril) versus norfloxacin in single dose for adult female uncomplicated UTIs. Multicenter randomized, double-blind study. Chemotherapy 1990; 36Suppl 1: 31–3
Van Pienbroek E, Hermans J, Kaptein AA, et al. Fosfomycin trometamol in a single dose versus seven days nitrofurantoin in the treatment of acute uncomplicated urinary tract infections in women. Pharm World Sci 1993 Dec 17; 15: 257–62
Data on file. Update of efficacy and safety information MON-US-01, MON-US-02, MON-US-03. Forest Laboratories, Inc. USA. 1996
Data on file. MON-US-03: single dose fosfomycin tromethamine versus multiple dose nitrofurantoin monohydrate/macrocrystals for the treatment of uncomplicated urinary tract infections in female patients. Forest Laboratories, Inc. USA. 1996
Rubin RH, Shapiro ED, Andriole VT, et al. Evaluation of new anti-infective drugs for the treatment of urinary tract infection. Clin Infect Dis 1992; 15Suppl. 1: S216–27
Moroni M. Monuril in lower uncomplicated urinary tract infections in adults. Eur Urol 1987; 13Suppl. 1: 101–4
Romero R, Oyarzun E, Mazor M, et al. Meta-analysis of the relationship between asymptomatic bacteriuria and preterm delivery/low birth weight. Obstet Gynecol 1989 April; 73(4): 576–82
Reeves DS. Treatment of bacteriuria in pregnancy with single dose fosfomycin trometamol: a review. Infection 1992; 20Suppl. 4: S 313–6
Bailey RR. Single-dose antibacterial treatment for bacteriuria in pregnancy. Drugs 1984; 27: 183–6
Thoumsin H, Aghayan M, Lambotte R. Single dose fosfomycin trometamol versus multiple dose nitrofurantoin in pregnant women with bacteriuria: preliminary results. Infection 1990; 18Suppl. 2: 94–7
Principi N, Corda R, Bassetti D, et al. Fosfomycin trometamol versus netilmicin in children’s lower urinary tract infections. Chemotherapy 1990; 36Suppl 1: 41–5
Peratoner L, Corrias A, Tumbarello R, et al. Fosfomycin trometamol versus netilmicin in pediatric urinary tract infections. A randomized multicenter study. In: Neu HC, Williams JD, editors. New trends in urinary tract infections. Basel: Karger, 1988: 171–7
Careddu P, Borzani M, Scotti L, et al. Treatment of lower urinary tract infections in children: single dose fosfomycin trometamol versus pipemidic acid. Chemioterapia 1987 Aug; 6: 290–4
Naber KG, Johnson FN. The safety and tolerability of fosfomycin trometamol. Rev Contemp Pharmacother 1995; 6(2): 63–70
Stamm WE. Single dose treatment of urinary tract infections: an overview. In: Bailey RR, editor. Single dose therapy of urinary tract infections. 1st ed. Sydney: Adis Health Science Press, 1983: 98–106
Naber KG. Uncomplicated urinary tract infections — is single-dose therapy effective? Int J Antimicrob Agents 1994; 4Suppl. 2: 39–45
Bailey RR. Review of published studies on single dose therapy of urinary tract infections. Infection 1990; 18Suppl. 2: S53–6
Plumridge RJ, Golledge CL. Treatment of urinary tract infection. Clinical and economic considerations. Pharmaco-economics 1996; 9(4): 295–306
Gatley MS. To be taken as directed. J R Coll Gen Pract 1968; 16: 39–44
Cunha BA. The importance of compliance with oral antibiotic regimens. Adv Ther 1988; 5(6): 297–305
Grob PR. Antibiotic prescribing practices and patient compliance in the community. Scand J Infect Dis 1992 Suppl. 83: 7–14
Sanson-Fisher R, Bowman J, Armstrong S. Factors affecting nonadherence with antibiotics. Diagn Microbiol Infect Dis 1992; 15: 103S–9S
Urquhart J. Ascertaining how much compliance is enough with outpatient antibiotic regimens. Postgrad Med J 1992; 68Suppl. 3: S49–59
Sclar DA, Tartaglione TA, Fine MJ. Overview of issues related to medical compliance with implications for the outpatient management of infectious diseases. Infect Agent Dis 1994; 3(5): 266–73
Slack R, Greenwood D. The microbiological and pharmacokinetic profile of an antibacterial agent useful for the single-dose therapy of urinary tract infection. Eur Urol 1987; 13Suppl 1: 32–6
Forest Monurol single-dose UTI therapy will be launched in April. F-D-C Reports — The Pink Sheet. T&G 3. Dec 23 1996.
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: R.R. Bailey, Department of Nephrology, Christchurch Hospital, Christchurch, New Zealand; A.L. Barry, Clinical Microbiology Institute, Tualatin, Oregon, USA; T. Bergan, Institute of Medical Microbiology, University of Oslo, Oslo, Norway; E. Bergogne-Bérézin, Laboratoire de Microbiologie, C.H.U. Bichat, Paris, France; G.G. Grassi, Facoltà di Medicina e Chirurgia, Università di Pavia, Pavia, Italy; D. Greenwood, Department of Clinical Laboratory Sciences, University Hospital, Nottingham, England; J.M.T. Hamilton-Miller, Department of Medical Microbiology, The Royal Free Hospital School of Medicine, London, England; C.M. Kunin, University Hospitals Department of Internal Medicine, Ohio State University, Columbus, Ohio, USA; K.G. Naber, Urologische Klinik, Elisabeth-Krankenhaus, Straubing, Germany; W.G. Pittman, Ambulatory Center, Lloyd Noland Hospital and Health Centers, Fairfield, Alabama, USA; R. Raz, Infectious Diseases Unit, Central Emek Hospital, Afula, Israel; D.S. Reeves, Department of Medical Microbiology, Southmead Hospital, Bristol, England; G.C. Schito, Istituto di Microbiologia, Università Degli Studi di Genova, Genoa, Italy; S.H. Zinner, Department of Medicine, Brown University, Providence, Rhode Island, USA.
Rights and permissions
About this article
Cite this article
Patel, S.S., Balfour, J.A. & Bryson, H.M. Fosfomycin Tromethamine. Drugs 53, 637–656 (1997). https://doi.org/10.2165/00003495-199753040-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199753040-00007